Abstract
Neovascularization plays a critical role in cancer metastasis. However, the molecular mechanism regulating the neovascularization in oral squamous cell carcinoma (OSCC) is poorly understood. Placental growth factor (PLGF) has been known to regulate pathological angiogenesis and has been recently shown to regulate matrix metalloproteinases (MMPs) for extracellular matrix degradation during neovascularization. Here we aimed to examine whether PLGF may regulate MMPs in the metastasis of OSCC. We found that PLGF and MMP9 levels strongly correlated in OSCC in the patients, both increased in the OSCC from the patients with metastasis of the primary OSCC. Thus, we used several human OSCC cell lines to examine the relationship between PLGF and MMP9. We found that overexpression of PLGF in OSCC cells increased expression of MMP9, while inhibition of PLGF in OSCC cells decreased expression of MMP9. However, adaptation of MMP9 levels in OSCC cells did not affect the levels of PLGF. These data suggest that PLGF may regulate MMP9 in OSCC cells, but not vice versa. Moreover, inhibition of ERK1/2, but not inhibition of PI3k or JNK pathways, substantially abolished the effect of PLGF on MMP9, suggesting that PLGF may increase expression of MMP9 via ERK/MAPK signaling pathway. Thus, our data demonstrate that PLGF-induced cancer neovascularization may be partially mediated through its effect on MMP9 activation in OSCC.





Similar content being viewed by others
References
Bodner L, Manor E, Friger MD, van der Waal I. Oral squamous cell carcinoma in patients twenty years of age or younger—review and analysis of 186 reported cases. Oral Oncol. 2014;50:84–9.
Zafereo ME. Evaluation and staging of squamous cell carcinoma of the oral cavity and oropharynx: limitations despite technological breakthroughs. Otolaryngol Clin N Am. 2013;46:599–613.
Andisheh-Tadbir A, Khademi B, Kamali F, Fattahi MJ, Malekzadeh M, Taghva M. Upregulation of serum vascular endothelial growth factor and matrix metalloproteinase-3 in patients with oral squamous cell carcinoma. Tumour Biol. 2014;35:5689–93.
Zhang E, Liu S, Xu Z, Huang S, Tan X, Sun C, et al. Pituitary tumor-transforming gene 1 (PTTG1) is overexpressed in oral squamous cell carcinoma (OSCC) and promotes migration, invasion and epithelial-mesenchymal transition (EMT) in SCC15 cells. Tumour Biol. 2014;35:8801–11.
Dufour A, Overall CM. Missing the target: matrix metalloproteinase antitargets in inflammation and cancer. Trends Pharmacol Sci. 2013;34:233–42.
Dome B, Hendrix MJ, Paku S, Tovari J, Timar J. Alternative vascularization mechanisms in cancer: pathology and therapeutic implications. Am J Pathol. 2007;170:1–15.
Bhujwalla ZM, Artemov D, Aboagye E, Ackerstaff E, Gillies RJ, Natarajan K, et al. The physiological environment in cancer vascularization, invasion and metastasis. Novartis Found Symp. 2001;240:23–38. discussion 38–45, 152–153.
Davidson B, Reich R, Risberg B, Nesland JM. The biological role and regulation of matrix metalloproteinases (MMP) in cancer. Arkh Patol. 2002;64:47–53.
Rhee JS, Coussens LM. RECKing MMP function: implications for cancer development. Trends Cell Biol. 2002;12:209–11.
Vilen ST, Salo T, Sorsa T, Nyberg P. Fluctuating roles of matrix metalloproteinase-9 in oral squamous cell carcinoma. ScientificWorldJournal. 2013;2013:920595.
Mohtasham N, Anvari K, Memar B, Saghravanian N, Ghazi N, Bagherpour A, et al. Expression of e-cadherin and matrix metalloproteinase-9 in oral squamous cell carcinoma and histologically negative surgical margins and association with clinicopathological parameters. Rom J Morphol Embryol. 2014;55:117–21.
Oliveira LR, Castilho-Fernandes A, Oliveira-Costa JP, Soares FA, Zucoloto S, Ribeiro-Silva A: CD44+/CD133+ immunophenotype and matrix metalloproteinase-9: influence on prognosis in early-stage oral squamous cell carcinoma. Head Neck. 2013.
Ogbureke KU, Weinberger PM, Looney SW, Li L, Fisher LW. Expressions of matrix metalloproteinase-9 (MMP-9), dentin sialophosphoprotein (DSPP), and osteopontin (OPN) at histologically negative surgical margins may predict recurrence of oral squamous cell carcinoma. Oncotarget. 2012;3:286–98.
Elahi M, Rakhshan V, Ghasemian NT, Moshref M. Prognostic value of transforming growth factor beta 1 [TGF-beta1] and matrix metalloproteinase 9 [MMP-9] in oral squamous cell carcinoma. Biomarkers. 2012;17:21–7.
Liu CJ, Chang KW, Lin SC, Cheng HW. Presurgical serum levels of matrix metalloproteinase-9 and vascular endothelial growth factor in oral squamous cell carcinoma. Oral Oncol. 2009;45:920–5.
Tu HF, Wu CH, Kao SY, Liu CJ, Liu TY, Lui MT. Functional −1562 C-to-T polymorphism in matrix metalloproteinase-9 (MMP-9) promoter is associated with the risk for oral squamous cell carcinoma in younger male areca users. J Oral Pathol Med. 2007;36:409–14.
de Vicente JC, Fresno MF, Villalain L, Vega JA, Hernandez Vallejo G. Expression and clinical significance of matrix metalloproteinase-2 and matrix metalloproteinase-9 in oral squamous cell carcinoma. Oral Oncol. 2005;41:283–93.
Mukhopadhyay S, Munshi HG, Kambhampati S, Sassano A, Platanias LC, Stack MS. Calcium-induced matrix metalloproteinase 9 gene expression is differentially regulated by ERK1/2 and p38 MAPK in oral keratinocytes and oral squamous cell carcinoma. J Biol Chem. 2004;279:33139–46.
Tsai CH, Hsieh YS, Yang SF, Chou MY, Chang YC. Matrix metalloproteinase 2 and matrix metalloproteinase 9 expression in human oral squamous cell carcinoma and the effect of protein kinase C inhibitors: preliminary observations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:710–6.
Khan MH, Yasuda M, Higashino F, Haque S, Kohgo T, Nakamura M, et al. nm23-h1 suppresses invasion of oral squamous cell carcinoma-derived cell lines without modifying matrix metalloproteinase-2 and matrix metalloproteinase-9 expression. Am J Pathol. 2001;158:1785–91.
Ikebe T, Takeuchi H, Jimi E, Beppu M, Shinohara M, Shirasuna K. Involvement of proteasomes in migration and matrix metalloproteinase-9 production of oral squamous cell carcinoma. Int J Cancer. 1998;77:578–85.
Ferrara N. Vascular endothelial growth factor. Arterioscler Thromb Vasc Biol. 2009;29:789–91.
Xiao X, Prasadan K, Guo P, El-Gohary Y, Fischbach S, Wiersch J, et al. Pancreatic duct cells as a source of VEGF in mice. Diabetologia. 2014;57:991–1000.
Xiao X, Guo P, Chen Z, El-Gohary Y, Wiersch J, Gaffar I, et al. Hypoglycemia reduces vascular endothelial growth factor a production by pancreatic beta cells as a regulator of beta cell mass. J Biol Chem. 2013;288:8636–46.
Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–76.
Fischer C, Jonckx B, Mazzone M, Zacchigna S, Loges S, Pattarini L, et al. Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell. 2007;131:463–75.
Autiero M, Waltenberger J, Communi D, Kranz A, Moons L, Lambrechts D, et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nat Med. 2003;9:936–43.
Zhou X, Qi Y. PLGF inhibition impairs metastasis of larynx carcinoma through MMP3 downregulation. Tumour Biol. 2014;35:9381–6.
Biggs 3rd WH, Meisenhelder J, Hunter T, Cavenee WK, Arden KC. Protein kinase B/Akt-mediated phosphorylation promotes nuclear exclusion of the winged helix transcription factor FKHR1. Proc Natl Acad Sci U S A. 1999;96:7421–6.
Bagri A, Kouros-Mehr H, Leong KG, Plowman GD. Use of anti-VEGF adjuvant therapy in cancer: challenges and rationale. Trends Mol Med. 2010;16:122–32.
Acknowledgments
This work was supported by The Natural Science Foundation of Beijing City No. 7122161.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
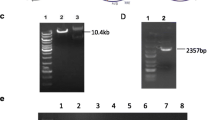
Supplementary Fig. 1
PLGF regulated MMP9 in OSCC cells. Human OSCC cell lines were transfected with either a PLGF-expressing plasmid (PLGF), or shPLGF, or null plasmid (−). Overexpression of PLGF in OSCC cells increased transcript levels of MMP9, while inhibition of PLGF in OSCC cells decreased transcript levels of MMP9. (PDF 33 kb)
Supplementary Fig. 2
PLGF was not regulated by MMP9. Human OSCC cell lines were transfected with either a MMP9-expressing plasmid (MMP9), or shMMP9, or a control null plasmid (−). Neither overexpression nor inhibition of MMP9 in OSCC cells altered the transcript levels of PLGF. (PDF 33 kb)
Rights and permissions
About this article
Cite this article
Bu, J., Bu, X., Liu, B. et al. Inhibition of metastasis of oral squamous cell carcinoma by anti-PLGF treatment. Tumor Biol. 36, 2695–2701 (2015). https://doi.org/10.1007/s13277-014-2892-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2892-y