Abstract
Background:
Adoptive therapy with tumour-infiltrating lymphocytes (TILs) induces durable complete responses (CR) in ∼20% of patients with metastatic melanoma. The recruitment of T cells through CXCR3/CCR5 chemokine ligands is critical for immune-mediated rejection. We postulated that polymorphisms and/or expression of CXCR3/CCR5 in TILs and the expression of their ligands in tumour influence the migration of TILs to tumours and tumour regression.
Methods:
Tumour-infiltrating lymphocytes from 142 metastatic melanoma patients enrolled in adoptive therapy trials were genotyped for CXCR3 rs2280964 and CCR5-Δ32 deletion, which encodes a protein not expressed on the cell surface. Expression of CXCR3/CCR5 in TILs and CXCR3/CCR5 and ligand genes in 113 available parental tumours was also assessed. Tumour-infiltrating lymphocyte data were validated by flow cytometry (N=50).
Results:
The full gene expression/polymorphism model, which includes CXCR3 and CCR5 expression data, CCR5-Δ32 polymorphism data and their interaction, was significantly associated with both CR and overall response (OR; P=0.0009, and P=0.007, respectively). More in detail, the predicted underexpression of both CXCR3 and CCR5 according to gene expression and polymorphism data (protein prediction model, PPM) was associated with response to therapy (odds ratio=6.16 and 2.32, for CR and OR, respectively). Flow cytometric analysis confirmed the PPM. Coordinate upregulation of CXCL9, CXCL10, CXCL11, and CCL5 in pretreatment tumour biopsies was associated with OR.
Conclusion:
Coordinate overexpression of CXCL9, CXCL10, CXCL11, and CCL5 in pretreatment tumours was associated with responsiveness to treatment. Conversely, CCR5-Δ32 polymorphism and CXCR3/CCR5 underexpression influence downregulation of the corresponding receptors in TILs and were associated with likelihood and degree of response.
Similar content being viewed by others
Main
Adoptive therapy with autologous tumour-infiltrating T lymphocytes (TILs) represents a promising treatment for patients with metastatic melanoma. In phase II trials, where TILs are expanded, activated ex vivo, and then adoptively transferred into patients in combination with systemic high-dose interleukin-(IL)-2 following lymphodepletion, durable complete responses (CR) were observed in ∼20% of patients (Rosenberg et al, 2011). However, the administration of preparative chemotherapy and high-dose IL-2 is associated with significant toxicity and no pretreatment biomarkers of responsiveness useful for patient selection are currently available.
Several studies in humans and animal models suggest that the recruitment of activated T lymphocytes through CXCR3 and CCR5 chemokine ligands has a key role immune-mediated tissue destruction, including tumour rejection (Wang et al, 2008; Bedognetti et al, 2010; Gajewski et al, 2011; Spivey et al, 2011; Gonzalez-Martin et al, 2012). We observed that systemically administered IL-2 induces inflammation within tumours leading to production of lymphocyte chemoattractants including CXCR3 and CCR5 ligands (Panelli et al, 2002; Panelli et al, 2004a; Bedognetti et al, 2010; Weiss et al, 2011). Indeed, the localisation of TILs within tumours is a necessary, although not sufficient, condition for tumour rejection (Pockaj et al, 1994). Thus, we postulated that polymorphisms and/or expression of CXCR3 and CCR5 may quantitatively and/or qualitatively influence chemokine receptor expression, and therefore influence migration of TILs to tumours and their regression.
The CCR5 polymorphism Δ32 consists of a 32-base deletion encoding a protein not expressed on the cell surface. Consequently, heterozygosity results in decreased and homozygosity absent receptor expression (Huang et al, 1996; Carrington et al, 1999). A retrospective study reported decreased survival of patients with metastatic melanoma carrying the CCR5-Δ32 polymorphism treated with immunotherapy (Ugurel et al, 2008). A common single nucleotide polymorphism (rs2280964) of CXCR3 has been recently associated with variation in receptor expression, lymphocyte chemotactic activity, and risk of developing asthma (Choi et al, 2008).
Here, in a prospective-retrospective hypothesis-driven analysis (Simon et al, 2009), we investigated the role of CXCR3 and CCR5 expression and polymorphisms (i.e., rs2280964 for CXCR3 and Δ32 for CCR5) by sequencing and profiling infused TILs from patients with metastatic melanoma undergoing adoptive therapy (N=142). Results were validated using flow cytometry (N=50). The role of CXCR3/CCR5 ligand gene expression was assessed by profiling matched pretreatment tumour biopsies (N=113).
Materials and methods
Patient samples
Samples from 142 patients were available: 142 TILs and 113 paired pretreatment tumour biopsies for RNA extraction, and 141 TILs for DNA extraction. Fifty paired TIL samples were also analysed using flow cytometry. Tumour-infiltrating lymphocytes were frozen just before the infusion. Samples were collected during five consecutive trials at the Surgery Branch, National Cancer Institute (Dudley et al, 2010; Rosenberg et al, 2011; Uccellini et al, 2012; http://www.clinicaltrials.gov/ct2/show/NCT00513604?term=07C0176&rank=1), codified as: TNMA, T200, T1200, TYT, and TCD8 (Table 1). All patients had progressive disease and had previously received standard or experimental regimens. Fifty percent of the patients (71 out of 142) achieved an objective response (OR), of which 25 (18%) experienced a durable CR and 46 (32%) a partial response (PR). Tumour biopsy samples included 24 CR (21%), 34 PR (30%) and 55 (49%) non-response (NR) samples.
Total body irradiation (TBI; 2 or 12 Gy) was administered in conjunction with chemotherapy in T200 and T1200 trials, respectively (Rosenberg et al, 2011). A day following lymphodepletion, TILs were infused into patients and high-dose IL-2 therapy was started. Protocols employed to generate TILs are described elsewhere (Dudley et al, 2003; Tran et al, 2008; Dudley et al, 2010; Rosenberg et al, 2011). Before TIL administration, patients received a non-myeloablative lymphodepleting regimen consisting of cyclophosphamide at 60 mg kg−1 per day for 2 days and fludarabine at 25 mg m−2 per day for 5 days (Dudley et al, 2010; Rosenberg et al, 2011). A day following lymphodepletion, TILs were infused into patients and high-dose IL-2 therapy was started (720 000 IU kg−1 intravenously every 8 h to tolerance). Major inclusion criteria included minimum age of 18 years, measurable disease, good clinical performance and life expectancy greater than 3 months. Detailed study protocol information are available elsewhere (http://www.clinicaltrials.gov/ct2/show/NCT00513604?term=07C0176&rank=1), (Dudley et al, 2010; Rosenberg et al, 2011).
All patients signed an informed consent approved by the Institutional Review Board of the National Cancer Institute. Data for this analysis are updated as of 11 January 2012. Response (CR, PR, or NR) was rated according to the Response Evaluation Criteria in Solid Tumors guidelines 4 weeks following TIL administration and at regular intervals thereafter. A CR or PR was considered an OR and a PR or NR was considered a non-CR.
Sequencing
DNA was successfully extracted from 141 TIL samples from frozen material (cell pellet) preserved at −80 °C. One sample was unavailable for DNA extraction. Total DNA was isolated with the Nucleic Acid Isolation System QuickGene-810 using the QuickGene DNA whole blood Mini Kit (Fujifilm, Tokyo, Japan).
Amplification PCR was carried out in a reaction mixture containing 4 μl (40 ng) of DNA, 10 μl of HotStar Taq Master Mix (Qiagen, Germantown, MD, USA), 1 μl (10 pmol) of each of the following primers: forward 5′-CTGGCCATCTCTGACCTGTT-3′ and reverse 5′-CCCTGTGCCTCTTCTTCTCA-3′ for CCR5 gene (Δ32 polymorphism) and forward 5′-CTCCCTACACTGAGGCTTGC-3′ and reverse 5′-AGCCATGGTCCTTGAGGTAA-3′ for CXCR3 gene (rs2280964 polymorphisms). Primers were designed using the Primer3 software (http://www.frodo.wi.mit.edu/). For CCR5 analysis, the reaction mixture was denatured at 95 °C for 10 min and cycled 35 times at 94 °C for 30 s, 58 °C for 30 s, and 72 °C for 60 s, with final extension at 72 °C for 10 min. For CXCR3 analysis, the reaction mixture was denatured at 95 °C for 10 min and cycled 32 times at 94 °C for 45 s, 58 °C for 45 s, and 72 °C for 60 s, with the final extension at 72 °C for 10 min.
The PCR product was purified with Exosap-IT (USB Corporation, Cleveland, OH, USA) according to the manufacturer’s protocol. PCR products were visualised on ultraviolet transilluminated, ethidium bromide 2% Agarose gel (Invitrogen, Carlsbad, CA, USA).
Sequencing reactions were performed using 3.5 μl of purified DNA product, 2 μl of Big Dye terminator (Big Dye Terminator v3.1 cycle sequencing reaction kit, Applied Biosystems, Foster City, CA, USA) and 4 pmol of forward primer. The following conditions were used: initial temperature of 96 °C for 60 s, followed by 30 cycles at 96 °C for 30 s, 50 °C for 30 s, and 60 °C for 4 min. Excess dye terminators were removed using DyeEx 96 Kit columns as per the manufacturer’s instructions (Qiagen).
The Sanger sequencing was performed on an ABI Prism 3730 XL instrument (Applied Biosystems). Data were analysed using Sequencher software v.4.9 (Gene Codes Corporation, Ann Arbor, MI, USA).
Samples for gene expression and sequencing experiments were processed in parallel during the same time period.
Gene expression
Total RNA was isolated from 142 TILs (cryopreserved just before the infusion into the patients) and 113 snap frozen tumour samples used for TIL generation. Total RNA was extracted with the Qiagen miRNeasy Mini kit and its quality was tested with the Agilent Bioanalyzer 2000 (Agilent Technologies, Palo Alto, CA, USA). Three hundred nanograms of total RNA were used for RNA amplification according to the manufacturer’s instructions (WT Expression Kit; Ambion, Austin, TX, USA). Amplified RNA was reverse transcribed into cDNAs followed by fragmentation. After hybridisation to the GeneChip Human Gene 1.0 ST Arrays, the chips were labelled with a WT Terminal Labeling Kit (Affymetrix, Santa Clara, CA, USA) and scanned on a GeneChip Scanner 3000 7G (Affymetrix). Data were normalised using the Robust Multi-Chip Average method and Log2-transformed using Partek Genomics Suite 6.4 (Partek Inc., St Louis, MO, USA). Data analyses were based on the whole transcripts.
Flow cytometry
Flow cytometry was performed in 50 TIL samples (cryopreserved just before the infusion into the patients) to validate the accuracy of genomic data in predicting cell surface protein expression. Tumour-infiltrating lymphocytes were selected as follows: (a) all available CRs; (2) samples concomitantly under- or overexpressing CXCR3 and CCR5; (3) CCR5-Δ32 homozygous samples; and (4) CCR5-Δ32 heterozygous samples included in the protein prediction model (PPM; described in the Results section). Because of the non-random sampling (selection bias), a correlation analysis between receptor expression and response was neither planned nor performed. Tumour-infiltrating lymphocyte samples included 18 CR (11 CXCR3/CCR5 low and 7 CXCR3/CCR5 high), 3 PR (CXCR3/CCR5 high) and 29 NR (14 CXCR3/CCR5 low and 15 CXCR3/CCR5 high) cases. Ten CCR5-Δ32 heterozygous (six PR, two CR and two NR) and one CCR5-Δ32 homozygous samples were selected, including six samples that were reclassified as the low group according to the PPM. Tumour-infiltrating lymphocytes preserved in liquid nitrogen were thawed, washed, immediately stained and analysed. FITC-labelled anti-CCR5 and PE-labelled anti-CXCR3 antibodies were used for chemokine receptor expression analyses. 7AAD antibodies were used to identify dead cells allowing for gating and analysis of live cells only. Samples were also stained with the appropriate isotype controls. Cells were analysed on a FACSCalibur flow cytometer (Becton Dickinson & Co, San Jose, CA, USA). Thirty thousand events were acquired on the FACSCalibur from each of the TIL samples for analysis. Daily fluctuations of the FACSCalibur flow cytometer were controlled by using Sphero 8 peak Rainbow Calibration Particles (Becton Dickinson & Co) and specific fluorescencent signal were calculated on the live cells by normalising to the appropriate isotype control, as described elsewhere (Pos et al, 2010). All of the antibodies were from Becton Dickinson & Co. Samples were stained according to the manufacturer’s protocols.
Statistical analysis
The difference of the overall outcome distribution (CR, PR, and NR) among CXCR3 and CCR5 polymorphism classes was assessed using the Kruskal–Wallis test that accounts for the ordered nature of the outcomes (i.e., degree of response: CR better than PR better than NR). The distribution of OR and CR between CXCR3 and CCR5 classes was then assessed by the χ2-test or Fisher’s exact test, as appropriate (i.e., if any category has a cell count <5). Odds ratios with their 95% CI were also reported, as appropriate. To minimise ‘data overfitting biases’, statistical significance levels and confidence intervals are not reported for data-derived hypotheses. As for the CXCR3 rs2280964 polymorphism, the four G carriers were not included in the genotype-response and genotype-transcript level correlation analysis. The associations between the expression of CXCR3 and CCR5 in TILs and clinical responses were first assessed individually by the Spearman rank correlation coefficient (ρ) tests, which account for the ordered nature of the outcomes. One sample was unavailable for genotyping. Logistic regression models were used to assess the joint association between the expression of CXCR3 and CCR5, the CCR5-Δ32 polymorphism, and their interactions with the clinical outcome, defined as either CR or OR. The log likelihood ratio test to was used to compare the fit of two models, one of which (the null model) is a special case of the other (the alternative model). The test is based on the log likelihood ratio, which expresses how many times more likely the data are under one model than the other. The null distribution of log likelihood is generated by calculating the log likelihood for each permutation. The variables included in the model are defined as follows: X1, X2, X3 are binary variables; X1=1 when Log2 gene expression value of CCR5>median; X1=0 when Log2 gene expression value of CCR5⩽median; X2=1 when Log2 base gene expression value of CXCR3>median; X2=0 when Log2 base gene expression value of CXCR3⩽median; X3=0 when CCR5 polymorphism Δ32 is present; wild-type (WT)=1; Rx=treatment (TNMA, T200, T1200, TYT, and TCD8); Y: end point (CR or OR). During the model fitting, the sample with missing genotype data was omitted.
The gene expression model included CXCR3 and CCR5 expression and their interaction (model A). The gene expression/polymorphism model included CXCR3 and CCR5 expression, CCR5-Δ32 polymorphism, and their interaction (model B). Likelihood ratio tests were used to evaluate the statistical significance of effects in the models compared. The gene expression and the gene expression/polymorphism models were also controlled for treatment effect by including treatment variables in the two models (model C and model D, respectively).
In order to facilitate interpretation of the statistically significant interactions found in the logistic regression models, CXCR3 and CCR5 expression data were then dichotomised (low vs high) according to their respective median values and integrated with each other and with CCR5-Δ32 polymorphism data, resulting in a PPM.
Univariate associations between TIL and tumour CXCR3 and CCR5 expression and their polymorphisms were assessed by Student’s t-test (CCR5-Δ32 polymorphism) after checking for normal distribution (the D′Agostino–Pearson normality test) or by the Spearman rank correlation coefficient (ρ) test (CXCR3 rs2280964 polymorphism). Association between sex, age and clinical outcomes (CR or OR), as well as cluster enrichment analysis was assessed by the χ2- or Fisher exact test, as appropriate.
Correlation between flow cytometry and gene expression data was assessed by the Spearman rank correlation coefficient (ρ) test as flow cytometry data were not normally distributed.
The correlation matrix of tumour biopsy gene expression data was based on the Spearman rank correlation coefficient (ρ) test because not all the data were normally distributed. Hierarchical clustering was based on the Euclidean distances, and was performed with Partek Genomics Suite 6.4. Probability (P) values <0.05 (two-sided) were considered to be statistically significant. All statistical tests were two sided. Analyses were performed with SPSS version 18.0 (SPSS, Chicago, IL, USA), Partek Genomics Suite 6.4 (Partek Inc., and R (Bedognetti et al, 2011).
Single subject CXCR3 rs2280964 genotypes (HapMap and 1000 Genome Projects, CEU populations) were downloaded from ensembl (http://www.useast.ensembl.org/index.html).
Results
Tumour-infiltrating lymphocyte sequencing
Demographic characteristics of the study population are shown in Table 1. As for CXCR3 (located on the X chromosome), no association was observed between response and rs2280964 genotype (Table 2). The frequencies of T allele were 0.24 and 0.30 in men and women, respectively. These frequencies are similar to those reported in individuals with European ancestry (T-allele frequency in men: 0.26 and 0.20, CEU HapMap, and CEU 1000 Genomes Project, respectively; T-allele frequency in women: 0.22 and 0.27, CEU HapMap, and CEU 1000 Genomes Project, respectively). Interestingly, we found four men (one CR, two PR, and one NR) carrying the G allele (electopherograms in Supplementary Figure S1). Although rs2280964 is annotated as bi-allelic (C/T) polymorphism in the dbSNP database (http://www.ncbi.nlm.nih.gov/snp/?term=2280964), HapMap project and genome-wide association studies (both array based) might miss the identification of tri-allelic variants (Ellinghaus et al, 2009). In fact, array-based genotyping need the knowledge of a third allele being present for the assays design, otherwise the third allele cannot be detected without using appropriate imputation algorithms (Huebner et al, 2007). However, programs used to genotype the current phase 1 release of 1000 Genomes Projects (sequencing based) are unable to genotype sites with more than two alleles. (http://www.1000genomes.org/faq/are-all-genotype-calls-current-release-vcf-files-bi-allelic).
As for CCR5, the frequency of the Δ32 genotype is ∼20% in Caucasians (Carrington et al, 1999). Similarly, we found 26 patients (18.4%) carrying the Δ32 polymorphism (1 homozygous and 25 heterozygous). The difference in the overall distribution of the outcomes for the WT and Δ32 patients was borderline significant (P=0.058) when checked with the Kruskal–Wallis test that assumes a progressive enrichment of one genotype over the other in three ordered response classes (i.e., CR>PR>NR). Although the CR rate was similar between the two groups (24% vs 16%), 17 of 25 patients (68%) carrying the Δ32 polymorphism (including the homozygous patients) experienced an OR, whereas only 53 of 116 (46%) WT patients experienced an OR (odds ratio=2.53, CI=1.01–6.32, Δ32 vs WT patients, respectively, P=0.043, Table 2).
Tumour-infiltrating lymphocyte gene expression and integrated gene expression and sequencing analysis
No differences in CXCR3 and CCR5 expression in TILs among the response classes was observed when data were compared by the Spearman rank correlation coefficient (ρ) test, which assumes a progressive change in gene expression in the three ordered response classes (i.e., CR>PR>NR or CR<PR<NR), having CR and PR samples the lowest and the highest transcript levels (CXCR3 and CCR5 gene expression data distribution is shown in Supplementary Figure S2).
To evaluate the weight on response of the coordinate expression of CXCR3 and CCR5, which have redundant functions, we utilised logistic regression analyses (Table 3). The gene expression model with interaction (full A model), included as predictor variables the expression of the two genes in TILs and the two-way interaction between the individual gene expressions. This model was significantly associated with CR (P=0.032) but not significantly associated with OR (P=0.15). The gene expression/polymorphism model with interaction (full B model) includes the variables of the full A model as well as an indicator variable for Δ32 polymorphism and the two-way and three way interaction of the CCR5-Δ32 polymorphism with the gene expression variables. By adding the DNA dimension (CCR5-Δ32 polymorphism), the model was significantly associated with both CR (P=0.0009) and OR (P=0.007). The gene expression/polymorphism model with interaction (full B model) performed significantly better than the gene expression model with interaction (full A model) for both CR (P=0.003) and OR (P=0.007). As we detected a significant difference in OR and CR rates across the cohorts (see demographic characteristics in Table 1), we also evaluated models containing a treatment group factor, as well as the other variables. With this adjustment (model C and D), the gene expression model with interaction (full C model) remained significantly associated with CR (P=0.002), and became also significantly associated with OR (P=0.010). The gene expression/polymorphism model with interaction (full D model) remained significantly associated with CR (P=0.0001) and with OR (P=0.003) and, again, was significantly better than the gene expression model with interaction for CR and OR (P=0.005 and P=0.036, respectively). A detailed description of the results of the logistic regression models, including intermediate models, is reported in Supplementary Tables S1 and S2. Despite the possible intrinsic data overfitting, the employment of logistic models, which assess all the combination among the variables analysed, reduce biases related to the selection of group comparisons. Overall, these models clearly (and consistently) show that the addition of new dimensions to data (e.g., combinatorial gene expression analysis and integration with genetic polymorphisms) can increase the chances to identify patients more probably to respond to treatment.
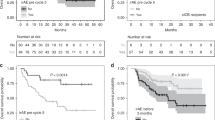
To understand the significant interactions identified by the logistic modelling, samples were grouped according to the expression of chemokine receptor genes. The CXCR3-low group was enriched in CR samples (CR rate: 25% vs 10%, odds ratio=3.11, CXCR3 low vs high, respectively, Figure 1A). The CCR5-low group was also slightly enriched in CR samples (CR rate: 21% vs 14%, odds ratio=1.63, CCR5 low vs high, respectively). Similar OR rate was observed in CXCR3-low group (as compared with CXCR3 high group), and in CCR5-low group (as compared with CCR5-high group, Figure 1B).
Effect of CXCR3/CCR5 expression status of tumor-infiltrating lymphocytes (TILs) on complete response ( A ) and objective response ( B). Odds ratios are represented. CCR5-Δ32 (DNA): presence of Δ32 polymorphism; CCR5-Δ32 low (PPM): CCR5 low according to the PPM (CCR5 below the median value according to the gene expression data or presence of CCR5-Δ32 polymorphism); CCR5 low (mRNA): CCR5 below the median value according to the gene expression data; CXCR3 low (RNA): CXCR3 below the median value according to the gene expression data; CXCR3/CCR5 low (mRNA): CXCR3 and CCR5 below the median value according to the gene expression data; CXCR3/CCR5 low (PPM): CXCR3 and CCR5 below the median value according to the gene expression data or CXCR3 low and CCR5 high in presence of CCR5-Δ32 polymorphism. P-values are from χ2-test. Abbreviations: CI=confidence interval; CR=complete response; non-CR=PR+NR; OR=objective response (CR+PR); PPM=protein prediction model; PR=partial response; WT=wild-type.
We then explored the coordinate underexpression of both transcripts. The samples with CXCR3 and CCR5 expression values below the median were grouped in the category CXCR3/CCR5 low (n=41) and those with at least one above the median were grouped as CXCR3/CCR5 high (n=101). Co-underexpression of both genes was strongly associated with achievement of CR: 32% of patients in the CXCR3/CCR5-low group achieved a CR compared with 12% in the CXCR3/CCR5-high group (odds ratio=3.44, Figure 1A). A similar trend was observed in the OR analysis (Figure 1B).
As the protein expression of CCR5 on TIL cell surface was expected to be reduced in CCR5-Δ32 patients (partially in heterozygous, complete in homozygous), we integrated this variable (i.e., CCR5-Δ32 polymorphism) with gene expression values to build a PPM. In the PPM (rational explained in detail in Figure 2), CCR5-Δ32 carriers with high CCR5 transcript levels (CCR5 high) were included in the CCR5-low (PPM) group and in the CXCR3/CCR5-low (PPM) group if CXCR3 was low. By adding this dimension, the disproportion of CR and OR samples between the CXCR3/CCR5-low vs -high group (PPM) increased (CR rate: 36% vs 8%, odds ratio=6.16; OR rate 64% vs 43%, odds ratio=2.32, CXCR3/CCR5 low vs high (PPM), respectively).
Protein prediction model. In wild-type subjects (A) we assume that high levels of CCR5 transcript are associated with high expression of CCR5 on cell surface. However, because Δ32 polymorphism encodes a protein not expressed on the cell surface (B), CCR5-Δ32 carriers were expected to have a low receptor expression (decreased in heterozygous individuals and absent in homozygous individuals) despite the high transcript expression.
No association was observed between expression of CXCR3 or CCR5 and the corresponding polymorphism in TILs or in tumour samples (Supplementary Figure S3).
Tumour-infiltrating lymphocyte flow cytometry
We validated the correlation between transcript and protein level in 50 available TIL samples (Figure 3). All TIL samples displayed strong, although variable, expression of CXCR3. CCR5 expression was weaker. The fluorescence intensity curve of the two chemokine receptors assumed a skewed Gaussian distribution without the evidence of well-defined subpopulations. Protein expression of CXCR3 correlated with the expression of their respective transcripts (Figure 3A). CCR5 transcript expression and CCR5 protein expression correlated in both WT and Δ32 samples (Figure 3E and F). CCR5-Δ32 strongly influenced the expression of CCR5 protein. The lower expression of CCR5 protein in CCR5-Δ32 in monocytes and T cells from CCR5-Δ32 carriers has been previously demonstrated (Carrington et al, 1999), but no data are available (to the best of our knowledge) on TILs. In fact, TILs used for adoptive therapy are cultured and expanded in vitro with consequent possible modulation of surface markers. We observed that the level of CCR5 receptor in CCR5-Δ32 heterozygous samples expressing high levels of CCR5 transcripts was approximately the half of that detected in CCR5 WT samples (Figure 3D). No expression of CCR5 receptor on cell surface was observed (as expected) in the CCR5-Δ32 homozygous sample. Therefore, even if post-transcriptional changes could influence the expression of CCR5 receptor (Shimizu et al, 2009), the presence of Δ32 polymorphism has a major role in lowering the expression of CCR5 protein in presence of high CCR5 transcripts in TILs.
Correlation between CXCR3/CCR5 transcript and protein expression in tumour-infiltrating lymphocytes (TILs). (A) Scatter plot representing the Spearman correlations between CXCR3 transcript (Log2 intensity, x axis) and protein expression (Fsp, y axis). (B) Overlaid histograms representing three representative CR samples with low level of CXCR3 transcript and receptor expression, and three NR samples with high level of CXCR3 transcript and receptor expression (according to the median value). Each sample is stained with CXCR3-PE (light blue graph) or with the corresponding IC (red graph). (C) Box plots showing the comparisons between samples with different CCR5 expression values (low and high according to the median value based on gene expression) and CCR5-Δ32 status (x axes): (D) Overlaid histograms exhibiting three representative CR samples with low level of CCR5 transcript and receptor expression and three NR samples with high level of CCR5 receptor expression (according to the median value). CR panel includes two CCR5 wild-type samples and one CCR5-Δ32 heterozygous sample. NR panel includes three CCR5 wild-type samples. Each sample is stained with CCR5-FITC (light blue graph) or with the corresponding IC (red graph). (E, F) Scatter plots representing the Spearman correlations between CCR5 transcript (Log2 intensity, x axis) and protein expression (Fsp, y axis) within all the samples (E) or within the CCR5-Δ32 heterozygous samples (F). Box plots: the top and the bottom edge of the tinted boxes show the values of the upper and lower quartiles, respectively. The top and the end of the whiskers represent the maximum and the minimum values excluding the outliers (which are plotted as individual dots). The horizontal lines indicate the median value. Specific fluorescent signal (Fsp) was calculated on live cells (7AAD negative) by normalising to the respective isotype control. Abbreviations: Δ32 Het mRNA low=CCR5-Δ32 heterozygous and CCR5 mRNA low; Δ32 Het mRNA high=CCR5-Δ32 heterozygous and CCR5 mRNA high; Δ32 Hom=CCR5-Δ32 homozygous; CR=complete response; PR=partial response; WT mRNA low=CCR5 wild-type and CCR5 mRNA low; WT mRNA high=CCR5 wild-type and CCR5 mRNA low; y axis represents CCR5-specific fluorescence signal (Fsp). P-values are from the Spearman rank correlation coefficient (ρ) test.
Despite the bias selection (see Materials and Methods section), it is noteworthy that only 1 out of 18 CR samples overexpressed both chemokine receptors (Figure 4). Thus, flow cytometry confirmed the PPM suggesting that estimates based on germ line and transcriptional data could be extended to the remaining samples for which TILs were no longer available.
Flow cytometry analysis of CXCR3 and CCR5 receptor expression by tumour-infiltrating lymphocytes (TILs). (A) Scatter plot of CXCR3 and CCR5 protein expression on cells surface. x axis: CCR5-specific fluorescent signal (Fsp); y axis: CXCR3-specific fluorescent signal (Fsp). Vertical and horizontal dotted lines represent the median values of the x and y axes, respectively. CR samples are represented with red dots, PR samples with green dots and NR samples with blue dots. The short grey arrows indicate CCR5-Δ32 heterozygous sample and the long grey arrow indicates the CCR5-Δ32 homozygous sample. (B) Flow cytometry scatter plots of three representative CR samples with low levels of CXCR3 and CCR5 transcript and receptor expression and three NR samples with high level of CXCR3 and CCR5 transcript and receptor expression (according to the median value) are represented. CR panel includes two CCR5 wild-type samples and one CCR5-Δ32 heterozygous sample. NR panel includes three CCR5 wild-type samples. Each sample was stained with CXCR3-PE and CCR5-FITC (light blue dots) or with the corresponding IC (red dots). CXCR3 and CCR5 gene expression status and CCR5 polymorphism is indicated for each sample. Specific fluorescent signal was calculated on live cells (7AAD negative) by normalising to the respective IC. Abbreviations: CR=complete response; IC=isotype control; OR=objective response (CR+PR); PR=partial response.
Pretreatment tumour biopsy gene expression
We investigated the role of the coordinate intratumoral expression of CXCR3/CXCR3 ligand gene expression (i.e., CXCL9, CXCL10, and CXCL11) and CCR5/CCR5 ligands (i.e., CCL3, CCL4, and CCL5) in 113 available pretreatment tumour biopsies used for TIL generation.
CXCL9, CXCL10, CXCL11 and CCL5 were co-expressed (Figure 5A) and, when used for hierarchical clustering analysis based on mean-centered expression values (Figure 5B), segregated melanoma metastases into three main groups: cluster 1 included samples with low CXCR3 and CCR5 ligand gene expression; cluster 2 and cluster 3 with intermediate and high expression, respectively. Cluster 1 was disproportionately enriched with samples from NR patients (OR rate: 38%, P=0.030) and cluster 3 with samples from OR patients (OR rate: 65%, P=0.031), whereas cluster 2 included an intermediate proportion of OR samples (52%), suggesting an association between expression of CXCL9, CXCL10, CXCL11 and CCL5 and immune responsiveness. CXCL9, CXCL10, CXCL11 and CCL5 are the classical interferon inducible chemokines and are coordinately regulated by STAT1 signalling (Chandrasekar et al, 2013; Rauch et al, 2013). No correlation with CR or OR was observed when samples were clustered according to the other markers (i.e., CCL3, CCL4, CXCR3, and CCR5, Supplementary Figure S4).
CXCR3/CCR5 ligands gene expression in pretreatment biopsies. (A) Hierarchical clustering of gene–gene correlation from 113 pretreatment tumours. The Spearman rank correlation coefficient (ρ) was calculated between combination of CXCR3, CCR5, CXCR3 ligands (CXCL9, CXCL10, and CXCL11) and CCR5 ligands (CCL3, CCL4, and CCL5). CXCL9, CXCL10, CXCL11 and CCL5 clustered together and were selected for hierarchical clustering analysis based on the mean-centered gene expression values (B). Patients with clinical complete responses (CR) are shown in red, patients with partial remission (PR) are shown in green and non-responders (NR) are shown in blue. Abbreviations: non-CR=PR+NR; OR=objective response (CR+PR). P-values are from the χ2-test.
Discussion
Activated cytotoxic and helper-1 T cells express CXCR3 and CCR5 on cell surface (Franciszkiewicz et al, 2012). The intratumoral overexpression of CXCR3 and/or CCR5 ligand genes in primary tumours has been correlated with high density of T cells and reduced risk of relapse or death in the lung (CCL5; Moran et al, 2002), melanoma (CCL5, CXCL9, and CXCL10), ovarian, (CXCL9 and CCL5; Zhang et al, 2003; Leffers et al, 2010) colorectal (CCL5, CXCL9, and CXCL10; Mlecnik et al, 2010; Tosolini et al, 2011), and breast cancer (CCL5, CXCL9, and CXCL10; Ascierto et al, 2012; Curtis et al, 2012). Consistently, Messina et al (2012) recently reported a prolonged survival in metastatic melanoma patients bearing tumours overexpressing CCL3, CCL4, CCL5, CXCL9, CXCL10, and CXCL11 (Messina et al, 2012). In addition, these chemokine genes have been associated with a higher likelihood to respond to ipilimumab (CCL4, CCL5, CXCL9, CXCL10, and CXCL11; Ji et al, 2012) and MAGE-A3 vaccination (CXCL9, CXCL10 and CCL5; Ulloa-Montoya et al, 2013) (Wang et al, 2013a).
Testing pretreatment biopsies from 113 melanoma patients undergoing adoptive therapy, we observed that the coordinated activation of the classical interferon inducible chemokine CXCL9, CXCL10, CXCL11 and CCL5 (Rauch et al, 2013) progressively increases the probability of response to adoptive therapy. CXCL9, CXCL10 and CCL5 represent the chemokines most frequently associated with both favourable prognostic and predictive role (Galon et al, 2013). We proposed that these chemokines identify a specific cancer immune phenotype (‘Th1, interferon-driven phenotype’) associated with better prognosis and responsiveness to immune manipulations (Ascierto et al, 2011; Spivey et al, 2012; Galon et al, 2013; Murtas et al, 2013).
We hypothesised that adoptively transferred TILs should be most likely to be effective when expressing high levels of the corresponding chemokine receptors. Ugurel et al (2008) reported that metastatic melanoma patients who carried one or two CCR5-Δ32 alleles suffer worse survival following immunotherapy or immunochemotherapy. The results from the 142 TILs were in apparent contradiction with this hypothesis. The CXCR3/CCR5 expression status was opposite than predicted. CCR5-Δ32 polymorphism, and CCR5 and CXCR3 transcript underexpression in TILs were associated with downregulation of the corresponding receptors and higher likelihood (OR rate) and degree (CR rate) of response. The association with achievement of a CR is intriguing and particularly relevant as CR patients treated with adoptive therapy usually experience a extremely durable remission (up to 100% of overall survival at 3 years (Rosenberg et al, 2011)). The strength of the association with response progressively increased as CCR5 and CXCR3 expression data were combined and were integrated with CCR5 sequencing data, as indicated by the log likelihood test for models.
These counterintuitive and surprising results could be explained by the dynamics of TIL migration to the tumour in relation to concomitant IL-2 administration. Localisation of TILs to the tumour site is necessary for their antitumour activity (Pockaj et al, 1994). However, soon (2 h) after high-dose IL-2 administration, the infused TILs rapidly disappear from the circulation. They do not localise to tumour tissue and rather migrate to normal liver, lung, and spleen (Fisher et al, 1989). Migration to the tumour begins 24 or 48 h after IL-2 administration and increases over time during the following days (Fisher et al, 1989). However, concentrations of CCR5 and CXCR3 ligands (e.g., CCL3, CCL4, CXCL9, CXCL10 and CXCL11) increase immediately after IL-2 administration (Panelli et al, 2004b). Our previous genomic and proteomic studies suggest that IL-2 seems to exert its effect on the tumour site indirectly by inducing monocyte activation, followed by a delayed, dose-dependent release of chemoattractants such as CXCR3 and CCR5 ligands that recruit TILs only in the later stages of treatment (Panelli et al, 2002; Wang et al, 2002; Panelli et al, 2004b; Weiss et al, 2011). In fact, administration of IL-2 is followed by a rapid clearance of peripheral mononuclear cells, without any evidence of their migration to tumour metastases at early time points (Panelli et al, 2002), consistently with results from adoptive therapy studies (Pockaj et al, 1994). Several richly perfused organs including the lung and liver, populated with IL-2-receptor carrying cells, are probably the primary target of systemic IL-2 administration, and it is there where the inflammatory cytokine storm is probably initiated leading, among others, to the production of massive quantities of CXCR3 and/or CCR5 ligands. A significant association was reported with increased persistence of TILs in the circulation 1 month following treatment and likelihood of clinical response (Dudley et al, 2002; Rosenberg et al, 2011). It is tempting to hypothesise that a low expression of chemokine receptors by TILs in the acute phases of treatment might prevent their sequestration by extratumoral tissues and paradoxically allow their subsequent localisation to the tumour when the cytokine storm has subsided and the tumour remains the only tissue maintaining expression of chemokines. This hypothesis would be consistent with the favourable predictive weight that higher expression of CXCL9, CXCL10, CXCL11, and CCL5 in steady state conditions confers. The enhancement of the expression of these chemokines in tumour/tumour microenvironment could identify novel strategies for the improvement of current immunotherapies (Muthuswamy et al, 2012; Pescatori et al, 2013).
These ligands could modulate the tumour microenvironment in other ways, independently of the recruitment of T cells. CCR5 blockade, for example, has been demonstrated to enhance proliferation of xenografts from breast cancer cells bearing WT p53, and the presence of Δ32 polymorphism has been associated with higher risk of relapse in breast cancer patients with p53 WT tumours (Manes et al, 2003). Thus, the aforementioned observation of Ugurel et al (2008) only apparently clashes with our findings. As response rate was not assessed in that study, the Δ32 polymorphism mutation may have enhanced tumour growth through a direct effect on tumour biology (Manes et al, 2003), resulting in the observed poor survival in these patients (Ugurel et al, 2008). As in our study the presence of CCR5-Δ32 mutation was not associated with worse response (and rather, when considered as single parameter, it was marginally associated with better OR, P=0.043), it is likely that the direct modulation of CCR5 in cancer tumour cells has a little (if any) impact on the clinical outcome of patients undergoing adoptive therapy.
However, it is possible that aside from the adoptive transfer model, when activated CXCR3+/CCR5+ TILs are infused in combination with high-dose IL-2, during other treatments (e.g., combination of immunochemotherapy (Ugurel et al, 2008)), the proportional induction of the CXCR3 and CCR5 ligands following treatment is not as unbalanced as it is in our study.
Although we stress that our findings must be prospectively validated, the significance of our observation is supported by the fact that it does not come from a merely retrospective investigation. Retrospective investigations performed on archived specimens are often conducted independent of a specified protocol and are unfocused, with numerous patient subsets and end points (Simon et al, 2009). Our prospective-retrospective (Simon et al, 2009) investigation was rather designed to study specimens collected during prospective trials and specifically stored to preserve DNAs, mRNAs and proteins in order to perform the dedicated assays.
Animal models can provide important mechanistic insights into human diseases. Studies in mouse models employing adoptively transferred lymphocytes have emphasised a key role of the upregulation of CCR5 in TILs in mediating tumour rejection (Gonzalez-Martin et al, 2012). Our present study, however, fails to demonstrate that the downregulation of CCR5 in TIL is a detrimental factor in this setting in humans.
However, in view of the intrinsic limitations of the investigation (e.g., the possible data overfitting because of the use of regression models), our results should be considered exploratory and need to be validated by integrated quantitative PCR, sequencing, and flow cytometric analyses in an independent cohort of patients.
Considering the complexity of tumour–host interactions, we believe that only a prospective clinical translation study employing serial biopsies (i.e., pre- and post treatment) in different tissues and specifically designed to asses T-cell tumour trafficking in humans can conclusively confirm the hypotheses generated by our present report.
In conclusion, our study identified candidate biomarkers of immune responsiveness in this setting by applying a combinatorial multifactorial approach. In fact, none of the individual parameters assessed had predictive value alone, but the coordinated analysis of the two molecules corrected for the predicted function according to the genetic polymorphism yielded strong predictive value. This point proposes a paradigm shift for the identification of clinically relevant biomarkers in complex biological problems. The optimisation of this approach in genomic-scale models represents a future challenge (Wang et al, 2013b).
Change history
29 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ascierto ML, De Giorgi V, Liu QZ, Bedognetti D, Spivey TL, Murtas D, Uccellini L, Ayotte BD, Stroncek DF, Chouchane L, Manjili MH, Wang E, Marincola FM (2011) An immunologic portrait of cancer. J Transl Med 9: 146.
Ascierto ML, Kmieciak M, Idowu MO, Manjili R, Zhao Y, Grimes M, Dumur C, Wang E, Ramakrishnan V, Wang XY, Bear HD, Marincola FM, Manjili MH (2012) A signature of immune function genes associated with recurrence-free survival in breast cancer patients. Breast Cancer Res Treat 131 (3): 871–880.
Bedognetti D, Balwit JM, Wang E, Disis ML, Britten CM, Delogu LG, Tomei S, Fox BA, Gajewski TF, Marincola FM, Butterfield LH (2011) SITC/iSBTc cancer immunotherapy biomarkers resource document: online resources and useful tools—a compass in the land of biomarker discovery. J Transl Med 9: 155.
Bedognetti D, Wang E, Sertoli MR, Marincola FM (2010) Gene-expression profiling in vaccine therapy and immunotherapy for cancer. Expert Rev Vaccines 9 (6): 555–565.
Carrington M, Dean M, Martin MP, O′Brien SJ (1999) Genetics of HIV-1 infection: chemokine receptor CCR5 polymorphism and its consequences. Hum Mol Genet 8 (10): 1939–1945.
Chandrasekar B, Deobagkar-Lele M, Victor ES, Nandi D (2013) Regulation of chemokines, CCL3 and CCL4, by interferon gamma and nitric oxide synthase 2 in mouse macrophages and during Salmonella enterica serovar typhimurium infection. J Infect Dis 207 (10): 1556–1568.
Choi JW, Park CS, Hwang M, Nam HY, Chang HS, Park SG, Han BG, Kimm K, Kim HL, Oh B, Kim Y (2008) A common intronic variant of CXCR3 is functionally associated with gene expression levels and the polymorphic immune cell responses to stimuli. J Allergy Clin Immunol 122 (6): 1119–1126, e7.
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, Speed D, Lynch AG, Samarajiwa S, Yuan Y, Graf S, Ha G, Haffari G, Bashashati A, Russell R, McKinney S, Langerod A, Green A, Provenzano E, Wishart G, Pinder S, Watson P, Markowetz F, Murphy L, Ellis I, Purushotham A, Borresen-Dale AL, Brenton JD, Tavare S, Caldas C, Aparicio S (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486 (7403): 346–352.
Dudley ME, Gross CA, Langhan MM, Garcia MR, Sherry RM, Yang JC, Phan GQ, Kammula US, Hughes MS, Citrin DE, Restifo NP, Wunderlich JR, Prieto PA, Hong JJ, Langan RC, Zlott DA, Morton KE, White DE, Laurencot CM, Rosenberg SA (2010) CD8+ enriched ‘young’ tumor infiltrating lymphocytes can mediate regression of metastatic melanoma. Clin Cancer Res 16 (24): 6122–6131.
Dudley ME, Wunderlich JR, Robbins PF, Yang JC, Hwu P, Schwartzentruber DJ, Topalian SL, Sherry R, Restifo NP, Hubicki AM, Robinson MR, Raffeld M, Duray P, Seipp CA, Rogers-Freezer L, Morton KE, Mavroukakis SA, White DE, Rosenberg SA (2002) Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science 298 (5594): 850–854.
Dudley ME, Wunderlich JR, Shelton TE, Even J, Rosenberg SA (2003) Generation of tumor-infiltrating lymphocyte cultures for use in adoptive transfer therapy for melanoma patients. J Immunother 26 (4): 332–342.
Ellinghaus D, Schreiber S, Franke A, Nothnagel M (2009) Current software for genotype imputation. Hum Genomics 3 (4): 371–380.
Fisher B, Packard BS, Read EJ, Carrasquillo JA, Carter CS, Topalian SL, Yang JC, Yolles P, Larson SM, Rosenberg SA (1989) Tumor localization of adoptively transferred indium-111 labeled tumor infiltrating lymphocytes in patients with metastatic melanoma. J Clin Oncol 7 (2): 250–261.
Franciszkiewicz K, Boissonnas A, Boutet M, Combadiere C, Mami-Chouaib F (2012) Role of chemokines and chemokine receptors in shaping the effector phase of the antitumor immune response. Cancer Res 72 (24): 6325–6332.
Gajewski TF, Fuertes M, Spaapen R, Zheng Y, Kline J (2011) Molecular profiling to identify relevant immune resistance mechanisms in the tumor microenvironment. Curr Opin Immunol 23 (2): 286–292.
Galon J, Angell Helen K, Bedognetti D, Marincola Francesco M (2013) The continuum of cancer immunosurveillance: prognostic, predictive, and mechanistic signatures. Immunity 39 (1): 11–26.
Gonzalez-Martin A, Mira E, Manes S (2012) CCR5 in cancer immunotherapy: More than an ‘attractive’ receptor for T cells. Oncoimmunology 1 (1): 106–108.
Huang Y, Paxton WA, Wolinsky SM, Neumann AU, Zhang L, He T, Kang S, Ceradini D, Jin Z, Yazdanbakhsh K, Kunstman K, Erickson D, Dragon E, Landau NR, Phair J, Ho DD, Koup RA (1996) The role of a mutant CCR5 allele in HIV-1 transmission and disease progression. Nat Med 2 (11): 1240–1243.
Huebner C, Petermann I, Browning BL, Shelling AN, Ferguson LR (2007) Triallelic single nucleotide polymorphisms and genotyping error in genetic epidemiology studies: MDR1 (ABCB1) G2677/T/A as an example. Cancer Epidemiol Biomarkers Prev 16 (6): 1185–1192.
Ji RR, Chasalow SD, Wang L, Hamid O, Schmidt H, Cogswell J, Alaparthy S, Berman D, Jure-Kunkel M, Siemers NO, Jackson JR, Shahabi V (2012) An immune-active tumor microenvironment favors clinical response to ipilimumab. Cancer Immunol Immunother 61 (7): 1019–1031.
Leffers N, Fehrmann RS, Gooden MJ, Schulze UR, Ten Hoor KA, Hollema H, Boezen HM, Daemen T, de Jong S, Nijman HW, van der Zee AG (2010) Identification of genes and pathways associated with cytotoxic T lymphocyte infiltration of serous ovarian cancer. Br J Cancer 103 (5): 685–692.
Manes S, Mira E, Colomer R, Montero S, Real LM, Gomez-Mouton C, Jimenez-Baranda S, Garzon A, Lacalle RA, Harshman K, Ruiz A, Martinez AC (2003) CCR5 expression influences the progression of human breast cancer in a p53-dependent manner. J Exper Med 198 (9): 1381–1389.
Messina JL, Fenstermacher DA, Eschrich S, Qu X, Berglund AE, Lloyd MC, Schell MJ, Sondak VK, Weber JS, Mule JJ (2012) 12-chemokine gene signature identifies lymph node-like structures in melanoma: potential for patient selection for immunotherapy? Sci Rep 2: 765.
Mlecnik B, Tosolini M, Charoentong P, Kirilovsky A, Bindea G, Berger A, Camus M, Gillard M, Bruneval P, Fridman WH, Pages F, Trajanoski Z, Galon J (2010) Biomolecular network reconstruction identifies T-cell homing factors associated with survival in colorectal cancer. Gastroenterology 138 (4): 1429–1440.
Moran CJ, Arenberg DA, Huang CC, Giordano TJ, Thomas DG, Misek DE, Chen G, Iannettoni MD, Orringer MB, Hanash S, Beer DG (2002) RANTES expression is a predictor of survival in stage I lung adenocarcinoma. Clin Cancer Res 8 (12): 3803–3812.
Murtas D, Maric D, De Giorgi V, Reinboth J, Worschech A, Fetsch P, Filie A, Ascierto ML, Bedognetti D, Liu Q, Uccellini L, Chouchane L, Wang E, Marincola FM, Tomei S (2013) IRF-1 responsiveness to IFN-gamma predicts different cancer immune phenotypes. Br J Cancer 109 (1): 76–82.
Muthuswamy R, Berk E, Junecko BF, Zeh HJ, Zureikat AH, Normolle D, Luong TM, Reinhart TA, Bartlett DL, Kalinski P (2012) NF-kappaB hyperactivation in tumor tissues allows tumor-selective reprogramming of the chemokine microenvironment to enhance the recruitment of cytolytic T Effector cells. Cancer Res 72 (15): 3735–3743.
Panelli MC, Martin B, Nagorsen D, Wang E, Smith K, Monsurro V, Marincola FM (2004a) A genomic- and proteomic-based hypothesis on the eclectic effects of systemic interleukin-2 administration in the context of melanoma-specific immunization. Cells Tissues Organs 177 (3): 124–131.
Panelli MC, Wang E, Phan G, Puhlmann M, Miller L, Ohnmacht GA, Klein HG, Marincola FM (2002) Gene-expression profiling of the response of peripheral blood mononuclear cells and melanoma metastases to systemic IL-2 administration. Genome Biol 3 (7): RESEARCH0035.
Panelli MC, White R, Foster M, Martin B, Wang E, Smith K, Marincola FM (2004b) Forecasting the cytokine storm following systemic interleukin (IL)-2 administration. J Transl Med 2 (1): 17.
Pescatori M, Bedognetti D, Venturelli E, Menard-Moyon C, Bernardini C, Muresu E, Piana A, Maida G, Manetti R, Sgarrella F, Bianco A, Delogu LG (2013) Functionalized carbon nanotubes as immunomodulator systems. Biomaterials 34 (18): 4395–4403.
Pockaj BA, Sherry RM, Wei JP, Yannelli JR, Carter CS, Leitman SF, Carasquillo JA, Steinberg SM, Rosenberg SA, Yang JC (1994) Localization of 111indium-labeled tumor infiltrating lymphocytes to tumor in patients receiving adoptive immunotherapy. Augmentation with cyclophosphamide and correlation with response. Cancer 73 (6): 1731–1737.
Pos Z, Selleri S, Spivey TL, Wang JK, Liu H, Worschech A, Sabatino M, Monaco A, Leitman SF, Falus A, Wang E, Alter HJ, Marincola FM (2010) Genomic scale analysis of racial impact on response to IFN-alpha. Proc Natl Acad Sci USA 107 (2): 803–808.
Rauch I, Muller M, Decker T (2013) The regulation of inflammation by interferons and their STATs. JAK-STAT 2 (1): e23820–13.
Rosenberg SA, Yang JC, Sherry RM, Kammula US, Hughes MS, Phan GQ, Citrin DE, Restifo NP, Robbins PF, Wunderlich JR, Morton KE, Laurencot CM, Steinberg SM, White DE, Dudley ME (2011) Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res 17 (13): 4550–4557.
Shimizu S, Kamata M, Kittipongdaja P, Chen KN, Kim S, Pang S, Boyer J, Qin FX, An DS, Chen IS (2009) Characterization of a potent non-cytotoxic shRNA directed to the HIV-1 co-receptor CCR5. Genet Vaccines Ther 7: 8.
Simon RM, Paik S, Hayes DF (2009) Use of archived specimens in evaluation of prognostic and predictive biomarkers. J Natl Cancer Inst 101 (21): 1446–1452.
Spivey TL, De Giorgi V, Zhao YD, Bedognetti D, Pos Z, Liu QZ, Tomei S, Ascierto ML, Uccellini L, Reinboth J, Chouchane L, Stroncek DF, Wang E, Marincola FM (2012) The stable traits of melanoma genetics: an alternate approach to target discovery. BMC Genomics 13: 156.
Spivey TL, Uccellini L, Ascierto ML, Zoppoli G, De Giorgi V, Delogu LG, Engle AM, Thomas JM, Wang E, Marincola FM, Bedognetti D (2011) Gene expression profiling in acute allograft rejection: challenging the immunologic constant of rejection hypothesis. J Transl Med 9: 174.
Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, Berger A, Bruneval P, Fridman WH, Pages F, Galon J (2011) Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, th2, treg, th17) in patients with colorectal cancer. Cancer Res 71 (4): 1263–1271.
Tran KQ, Zhou J, Durflinger KH, Langhan MM, Shelton TE, Wunderlich JR, Robbins PF, Rosenberg SA, Dudley ME (2008) Minimally cultured tumor-infiltrating lymphocytes display optimal characteristics for adoptive cell therapy. J Immunother 31 (8): 742–751.
Uccellini L, De Giorgi V, Zhao Y, Tumaini B, Erdenebileg N, Dudley ME, Tomei S, Bedognetti D, Ascierto ML, Liu Q, Simon R, Kottyan L, Kaufman KM, Harley JB, Wang E, Rosenberg SA, Marincola FM (2012) IRF5 gene polymorphisms in melanoma. J Transl Med 10 (1): 170.
Ugurel S, Schrama D, Keller G, Schadendorf D, Brocker EB, Houben R, Zapatka M, Fink W, Kaufman HL, Becker JC (2008) Impact of the CCR5 gene polymorphism on the survival of metastatic melanoma patients receiving immunotherapy. Cancer Immunol Immunother 57 (5): 685–691.
Ulloa-Montoya F, Louahed J, Dizier B, Gruselle O, Spiessens B, Lehmann FF, Suciu S, Kruit WH, Eggermont AM, Vansteenkiste J, Brichard VG (2013) Predictive gene signature in MAGE-A3 antigen-specific cancer immunotherapy. J Clin Oncol 31 (19): 2388–2395.
Wang E, Bedognetti D, Marincola FM (2013a) Prediction of response to anticancer immunotherapy using gene signatures. J Clin Oncol 31 (19): 2369–2371.
Wang E, Bedognetti D, Tomei S, Marincola FM (2013b) Common pathways to tumor rejection. Ann N Y Acad Sci 1284 (1): 75–79.
Wang E, Miller LD, Ohnmacht GA, Mocellin S, Perez-Diez A, Petersen D, Zhao Y, Simon R, Powell JI, Asaki E, Alexander HR, Duray PH, Herlyn M, Restifo NP, Liu ET, Rosenberg SA, Marincola FM (2002) Prospective molecular profiling of melanoma metastases suggests classifiers of immune responsiveness. Cancer Res 62 (13): 3581–3586.
Wang E, Worschech A, Marincola FM (2008) The immunologic constant of rejection. Trends Immunol 29 (6): 256–262.
Weiss GR, Grosh WW, Chianese-Bullock KA, Zhao Y, Liu H, Slingluff CL Jr, Marincola FM, Wang E (2011) Molecular insights on the peripheral and intratumoral effects of systemic high-dose rIL-2 (aldesleukin) administration for the treatment of metastatic melanoma. Clin Cancer Res 17 (23): 7440–7450.
Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN, Rubin SC, Coukos G (2003) Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 348 (3): 203–213.
Acknowledgements
This study was supported by the Intramural Research program of the US National Institutes of Health and by the Conquer Cancer Foundation of the American Society of Clinical Oncology (2011 Young Investigator Award Grant, granted to Davide Bedognetti). Dr Bedognetti's fellowship was initially supported by the Italian Association of Medical Oncology (AIOM) Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bedognetti, D., Spivey, T., Zhao, Y. et al. CXCR3/CCR5 pathways in metastatic melanoma patients treated with adoptive therapy and interleukin-2. Br J Cancer 109, 2412–2423 (2013). https://doi.org/10.1038/bjc.2013.557
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.557
Keywords
This article is cited by
-
Germline modifiers of the tumor immune microenvironment implicate drivers of cancer risk and immunotherapy response
Nature Communications (2023)
-
The immune landscape of solid pediatric tumors
Journal of Experimental & Clinical Cancer Research (2022)
-
Cross-Platform Omics Prediction procedure: a statistical machine learning framework for wider implementation of precision medicine
npj Digital Medicine (2022)
-
Perspectives of tumor-infiltrating lymphocyte treatment in solid tumors
BMC Medicine (2021)
-
Optimal combination treatment regimens of vaccine and radiotherapy augment tumor-bearing host immunity
Communications Biology (2021)