Abstract
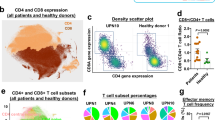
Delayed T cell recovery and restricted T cell receptor (TCR) diversity after allogeneic hematopoietic stem cell transplantation (allo-HSCT) are associated with increased risks of infection and cancer relapse. Technical challenges have limited faithful measurement of TCR diversity after allo-HSCT. Here we combined 5′ rapid amplification of complementary DNA ends PCR with deep sequencing to quantify TCR diversity in 28 recipients of allo-HSCT using a single oligonucleotide pair. Analysis of duplicate blood samples confirmed that we accurately determined the frequency of individual TCRs. After 6 months, cord blood–graft recipients approximated the TCR diversity of healthy individuals, whereas recipients of T cell–depleted peripheral-blood stem cell grafts had 28-fold and 14-fold lower CD4+ and CD8+ T cell diversities, respectively. After 12 months, these deficiencies had improved for the CD4+ but not the CD8+ T cell compartment. Overall, this method provides unprecedented views of T cell repertoire recovery after allo-HSCT and may identify patients at high risk of infection or relapse.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Storek, J. et al. Reconstitution of the immune system after hematopoietic stem cell transplantation in humans. Semin. Immunopathol. 30, 425–437 (2008).
Seggewiss, R. & Einsele, H. Immune reconstitution after allogeneic transplantation and expanding options for immunomodulation: an update. Blood 115, 3861–3868 (2010).
Deeg, H.J. & Socie, G. Malignancies after hematopoietic stem cell transplantation: many questions, some answers. Blood 91, 1833–1844 (1998).
Small, T.N. et al. Comparison of immune reconstitution after unrelated and related T-cell–depleted bone marrow transplantation: effect of patient age and donor leukocyte infusions. Blood 93, 467–480 (1999).
Maury, S. et al. Prolonged immune deficiency following allogeneic stem cell transplantation: risk factors and complications in adult patients. Br. J. Haematol. 115, 630–641 (2001).
Nikolich-Zugich, J., Slifka, M.K. & Messaoudi, I. The many important facets of T-cell repertoire diversity. Nat. Rev. Immunol. 4, 123–132 (2004).
Goldberg, G.L., Zakrzewski, J.L., Perales, M.A. & van den Brink, M.R. Clinical strategies to enhance T cell reconstitution. Semin. Immunol. 19, 289–296 (2007).
Dumont-Girard, F. et al. Reconstitution of the T-cell compartment after bone marrow transplantation: restoration of the repertoire by thymic emigrants. Blood 92, 4464–4471 (1998).
Douek, D.C. et al. Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution. Lancet 355, 1875–1881 (2000).
Roux, E. et al. Recovery of immune reactivity after T-cell–depleted bone marrow transplantation depends on thymic activity. Blood 96, 2299–2303 (2000).
Weinberg, K. et al. Factors affecting thymic function after allogeneic hematopoietic stem cell transplantation. Blood 97, 1458–1466 (2001).
Lynch, H.E. et al. Thymic involution and immune reconstitution. Trends Immunol. 30, 366–373 (2009).
Langerak, A.W. et al. Molecular and flow cytometric analysis of the Vβ repertoire for clonality assessment in mature TCRαβ T-cell proliferations. Blood 98, 165–173 (2001).
Gaspar, H.B. et al. Long-term persistence of a polyclonal T cell repertoire after gene therapy for X-linked severe combined immunodeficiency. Sci. Transl. Med. 3, 97ra79 (2011).
Gorski, J. et al. Circulating T cell repertoire complexity in normal individuals and bone marrow recipients analyzed by CDR3 size spectratyping. Correlation with immune status. J. Immunol. 152, 5109–5119 (1994).
Memon, S.A., Sportes, C., Flomerfelt, F.A., Gress, R.E. & Hakim, F.T. Quantitative analysis of T cell receptor diversity in clinical samples of human peripheral blood. J. Immunol. Methods 375, 84–92 (2012).
Verfuerth, S. et al. Longitudinal monitoring of immune reconstitution by CDR3 size spectratyping after T-cell–depleted allogeneic bone marrow transplant and the effect of donor lymphocyte infusions on T-cell repertoire. Blood 95, 3990–3995 (2000).
Wu, C.J. et al. Reconstitution of T-cell receptor repertoire diversity following T-cell depleted allogeneic bone marrow transplantation is related to hematopoietic chimerism. Blood 95, 352–359 (2000).
Talvensaari, K. et al. A broad T-cell repertoire diversity and an efficient thymic function indicate a favorable long-term immune reconstitution after cord blood stem cell transplantation. Blood 99, 1458–1464 (2002).
Wang, C. et al. High throughput sequencing reveals a complex pattern of dynamic interrelationships among human T cell subsets. Proc. Natl. Acad. Sci. USA 107, 1518–1523 (2010).
Klarenbeek, P.L. et al. Human T-cell memory consists mainly of unexpanded clones. Immunol. Lett. 133, 42–48 (2010).
Robins, H.S. et al. Overlap and effective size of the human CD8+ T cell receptor repertoire. Sci. Transl. Med. 2, 47ra64 (2010).
Sherwood, A.M. et al. Deep sequencing of the human TCRγ and TCRβ repertoires suggests that TCRβ rearranges after αβ and γδ T cell commitment. Sci. Transl. Med. 3, 90ra61 (2011).
Venturi, V. et al. A mechanism for TCR sharing between T cell subsets and individuals revealed by pyrosequencing. J. Immunol. 186, 4285–4294 (2011).
Warren, R.L. et al. Exhaustive T-cell repertoire sequencing of human peripheral blood samples reveals signatures of antigen selection and a directly measured repertoire size of at least 1 million clonotypes. Genome Res. 21, 790–797 (2011).
Benichou, J., Ben-Hamo, R., Louzoun, Y. & Efroni, S. Rep-Seq: uncovering the immunological repertoire through next-generation sequencing. Immunology 135, 183–191 (2012).
Ponce, D.M. et al. Reduced late mortality risk contributes to similar survival after double-unit cord blood transplantation compared with related and unrelated donor hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. 17, 1316–1326 (2011).
Jacobson, C.A. et al. Immune reconstitution after double umbilical cord blood stem cell transplantation: comparison with unrelated peripheral blood stem cell transplantation. Biol. Blood Marrow Transplant. 18, 565–574 (2012).
Schumacher, T.N., Gerlach, C. & van Heijst, J.W. Mapping the life histories of T cells. Nat. Rev. Immunol. 10, 621–631 (2010).
Nguyen, P. et al. Identification of errors introduced during high throughput sequencing of the T cell receptor repertoire. BMC Genomics 12, 106 (2011).
Venturi, V., Kedzierska, K., Turner, S.J., Doherty, P.C. & Davenport, M.P. Methods for comparing the diversity of samples of the T cell receptor repertoire. J. Immunol. Methods 321, 182–195 (2007).
Lim, A. et al. Frequent contribution of T cell clonotypes with public TCR features to the chronic response against a dominant EBV-derived epitope: application to direct detection of their molecular imprint on the human peripheral T cell repertoire. J. Immunol. 165, 2001–2011 (2000).
Sauter, C. et al. Serious infection risk and immune recovery after double-unit cord blood transplantation without antithymocyte globulin. Biol. Blood Marrow Transplant. 17, 1460–1471 (2011).
Jakubowski, A.A. et al. T cell depleted stem-cell transplantation for adults with hematologic malignancies: sustained engraftment of HLA-matched related donor grafts without the use of antithymocyte globulin. Blood 110, 4552–4559 (2007).
Bacigalupo, A. et al. Defining the intensity of conditioning regimens: working definitions. Biol. Blood Marrow Transplant. 15, 1628–1633 (2009).
Barker, J.N. et al. A “no-wash” albumin-dextran dilution strategy for cord blood unit thaw: high rate of engraftment and a low incidence of serious infusion reactions. Biol. Blood Marrow Transplant. 15, 1596–1602 (2009).
Rowlings, P.A. et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br. J. Haematol. 97, 855–864 (1997).
Filipovich, A.H. et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol. Blood Marrow Transplant. 11, 945–956 (2005).
Schloss, P.D. et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl. Environ. Microbiol. 75, 7537–7541 (2009).
Alamyar, E., Giudicelli, V., Li, S., Duroux, P. & Lefranc, M.P. IMGT/HighV-QUEST: the IMGT(R) web portal for immunoglobulin (IG) or antibody and T cell receptor (TR) analysis from NGS high throughput and deep sequencing. Immunome Res. 8, 26 (2012).
Acknowledgements
We thank all patients and healthy donors who volunteered to participate in this study. We thank G. Redelman-Sidi for collection of blood samples, I. Leiner for processing of blood samples, C. Ubeda-Morant for assistance with data analysis, J. Li and A. Viale of the Memorial Sloan-Kettering Cancer Center Genomics Core Laboratory for performing Roche/454 sequencing and R. Jenq for critical reading of the manuscript. This work was supported by the Netherlands Organisation for Scientific Research (NWO) (Rubicon fellowship to J.W.J.v.H.), the Asociación Española Contra el Cáncer (AECC) (PAO grant to I.C.), the US National Institutes of Health (NIH) (grants HL069929, CA023766, AI080455, AI100288 and AI101406 to M.R.M.v.d.B. and AI042135, AI039031 and CA023766 to E.G.P.) and The Tow Foundation (to E.G.P.). Additional support was received from the US Department of Defense (USAMRAA Award W81XWH-09-1-0294), the Radiation Effects Research Foundation (RERF-NIAID), The Lymphoma Foundation, Alex's Lemonade Stand, The Geoffrey Beene Cancer Research Center at Memorial Sloan-Kettering Cancer Center and The Susan and Peter Solomon Divisional Genomics Program (to M.R.M.v.d.B.), The Translational and Integrative Medicine Research Fund of Memorial Sloan-Kettering Cancer Center, Cycle for Survival, The New York Community Trust and When Everyone Survives (to M.A.P.) and The Experimental Therapeutics Center of Memorial Sloan-Kettering Cancer Center funded by W.H. Goodwin and A. Goodwin (to M.R.M.v.d.B. and M.A.P.).
Author information
Authors and Affiliations
Contributions
J.W.J.v.H. designed and performed the study, analyzed data and wrote the manuscript. I.C. collected clinical data. L.B.L. performed Roche/454 sequencing. D.W.S. compared naive and memory CD8+ T cells. G.D.W., A.M.R.G. and J.L.N. provided patient samples. M.R.M.v.d.B. designed and supervised the study. M.A.P. designed and supervised the study and provided patient samples. E.G.P. designed and supervised the study, analyzed data and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7 and Supplementary Table 1 (PDF 2841 kb)
Rights and permissions
About this article
Cite this article
van Heijst, J., Ceberio, I., Lipuma, L. et al. Quantitative assessment of T cell repertoire recovery after hematopoietic stem cell transplantation. Nat Med 19, 372–377 (2013). https://doi.org/10.1038/nm.3100
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3100
This article is cited by
-
Maternal dendritic cells influence fetal allograft response following murine in-utero hematopoietic stem cell transplantation
Stem Cell Research & Therapy (2023)
-
Features of repertoire diversity and gene expression in human cytotoxic T cells following allogeneic hematopoietic cell transplantation
Communications Biology (2021)
-
T cell receptor beta locus sequencing early post-allogeneic stem cell transplant identifies patients at risk of initial and recurrent cytomegalovirus infection
Bone Marrow Transplantation (2021)
-
T cell regeneration after immunological injury
Nature Reviews Immunology (2021)
-
The role of the thymus in allogeneic bone marrow transplantation and the recovery of the peripheral T-cell compartment
Seminars in Immunopathology (2021)