Abstract
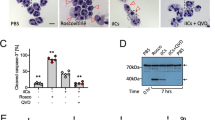
Neutrophil extracellular traps (NETs) are implicated in autoimmunity, but how they are generated and their roles in sterile inflammation remain unclear. Ribonucleoprotein immune complexes (RNP ICs), inducers of NETosis, require mitochondrial reactive oxygen species (ROS) for maximal NET stimulation. After RNP IC stimulation of neutrophils, mitochondria become hypopolarized and translocate to the cell surface. Extracellular release of oxidized mitochondrial DNA is proinflammatory in vitro, and when this DNA is injected into mice, it stimulates type I interferon (IFN) signaling through a pathway dependent on the DNA sensor STING. Mitochondrial ROS are also necessary for spontaneous NETosis of low-density granulocytes from individuals with systemic lupus erythematosus. This was also observed in individuals with chronic granulomatous disease, who lack NADPH oxidase activity but still develop autoimmunity and type I IFN signatures. Mitochondrial ROS inhibition in vivo reduces disease severity and type I IFN responses in a mouse model of lupus. Together, these findings highlight a role for mitochondria in the generation not only of NETs but also of pro-inflammatory oxidized mitochondrial DNA in autoimmune diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Nathan, C. Neutrophils and immunity: challenges and opportunities. Nat. Rev. Immunol. 6, 173–182 (2006).
Kolaczkowska, E. & Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat. Rev. Immunol. 13, 159–175 (2013).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 (2004).
Garcia-Romo, G.S. et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci. Transl. Med. 3, 73ra20 (2011).
Villanueva, E. et al. Netting neutrophils induce endothelial damage, infiltrate tissues and expose immunostimulatory molecules in systemic lupus erythematosus. J. Immunol. 187, 538–552 (2011).
Kahlenberg, J.M., Carmona-Rivera, C., Smith, C.K. & Kaplan, M.J. Neutrophil extracellular trap–associated protein activation of the NLRP3 inflammasome is enhanced in lupus macrophages. J. Immunol. 190, 1217–1226 (2013).
Lande, R. et al. Neutrophils activate plasmacytoid dendritic cells by releasing self-DNA–peptide complexes in systemic lupus erythematosus. Sci. Transl. Med. 3, 73ra19 (2011).
Denny, M.F. et al. A distinct subset of proinflammatory neutrophils isolated from patients with systemic lupus erythematosus induces vascular damage and synthesizes type I IFNs. J. Immunol. 184, 3284–3297 (2010).
Kaplan, M.J. Neutrophils in the pathogenesis and manifestations of SLE. Nat. Rev. Rheumatol. 7, 691–699 (2011).
Khandpur, R. et al. NETs are a source of citrullinated autoantigens and stimulate inflammatory responses in rheumatoid arthritis. Sci. Transl. Med. 5, 178ra40 (2013).
Knight, J.S. et al. Peptidylarginine deiminase inhibition is immunomodulatory and vasculoprotective in murine lupus. J. Clin. Invest. 123, 2981–2993 (2013).
Knight, J.S. et al. Peptidylarginine deiminase inhibition reduces vascular damage and modulates innate immune responses in murine models of atherosclerosis. Circ. Res. 114, 947–956 (2014).
Smith, C.K. et al. Neutrophil extracellular trap–derived enzymes oxidize high-density lipoprotein: an additional proatherogenic mechanism in systemic lupus erythematosus. Arthritis Rheumatol. 66, 2532–2544 (2014).
Knight, J.S., Carmona-Rivera, C. & Kaplan, M.J. Proteins derived from neutrophil extracellular traps may serve as self-antigens and mediate organ damage in autoimmune diseases. Front. Immunol. 3, 380 (2012).
Brinkmann, V. & Zychlinsky, A. Neutrophil extracellular traps: is immunity the second function of chromatin? J. Cell Biol. 198, 773–783 (2012).
Barrientos, L. et al. An improved strategy to recover large fragments of functional human neutrophil extracellular traps. Front. Immunol. 4, 166 (2013).
Wang, Y. et al. Histone hypercitrullination mediates chromatin decondensation and neutrophil extracellular trap formation. J. Cell Biol. 184, 205–213 (2009).
Holland, P.C. & Sherratt, H.S. Biochemical effects of the hypoglycemic compound diphenyleneiodonnium. Catalysis of anion–hydroxyl ion exchange across the inner membrane of rat liver mitochondria and effects on oxygen uptake. Biochem. J. 129, 39–54 (1972).
White, M.J. et al. Apoptotic caspases suppress mtDNA-induced STING-mediated type I IFN production. Cell 159, 1549–1562 (2014).
Oka, T. et al. Mitochondrial DNA that escapes from autophagy causes inflammation and heart failure. Nature 485, 251–255 (2012).
Shimada, K. et al. Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity 36, 401–414 (2012).
Altenhöfer, S., Radermacher, K.A., Kleikers, P.W., Wingler, K. & Schmidt, H.H. Evolution of NADPH oxidase inhibitors: selectivity and mechanisms for target engagement. Antioxid. Redox Signal. 23, 406–427 (2015).
Doughan, A.K., Harrison, D.G. & Dikalov, S.I. Molecular mechanisms of angiotensin II–mediated mitochondrial dysfunction: linking mitochondrial oxidative damage and vascular endothelial dysfunction. Circ. Res. 102, 488–496 (2008).
Dikalov, S. Cross-talk between mitochondria and NADPH oxidases. Free Radic. Biol. Med. 51, 1289–1301 (2011).
Mehta, P.K. & Griendling, K.K. Angiotensin II cell signaling: physiological and pathological effects in the cardiovascular system. Am. J. Physiol. Cell Physiol. 292, C82–C97 (2007).
Nakajima, A., Kurihara, H., Yagita, H., Okumura, K. & Nakano, H. Mitochondrial extrusion through the cytoplasmic vacuoles during cell death. J. Biol. Chem. 283, 24128–24135 (2008).
Gehrke, N. et al. Oxidative damage of DNA confers resistance to cytosolic nuclease TREX1 degradation and potentiates STING-dependent immune sensing. Immunity 39, 482–495 (2013).
Pazmandi, K. et al. Oxidative modification enhances the immunostimulatory effects of extracellular mitochondrial DNA on plasmacytoid dendritic cells. Free Radic. Biol. Med. 77, 281–290 (2014).
Ries, M. et al. Identification of novel oligonucleotides from mitochondrial DNA that spontaneously induce plasmacytoid dendritic cell activation. J. Leukoc. Biol. 94, 123–135 (2013).
Li, X. et al. Cyclic GMP–AMP synthase is activated by double-stranded DNA-induced oligomerization. Immunity 39, 1019–1031 (2013).
Remijsen, Q. et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 21, 290–304 (2011).
Kelkka, T. et al. Reactive oxygen species deficiency induces autoimmunity with type 1 interferon signature. Antioxid. Redox Signal. 21, 2231–2245 (2014).
Gergely, P. Jr. et al. Mitochondrial hyperpolarization and ATP depletion in patients with systemic lupus erythematosus. Arthritis Rheum. 46, 175–190 (2002).
Campbell, A.M., Kashgarian, M. & Shlomchik, M.J. NADPH oxidase inhibits the pathogenesis of systemic lupus erythematosus. Sci. Transl. Med. 4, 157ra141 (2012).
Bianchi, M. et al. Restoration of NET formation by gene therapy in CGD controls aspergillosis. Blood 114, 2619–2622 (2009).
Hultqvist, M., Olsson, L.M., Gelderman, K.A. & Holmdahl, R. The protective role of ROS in autoimmune disease. Trends Immunol. 30, 201–208 (2009).
Yu, E.P. & Bennett, M.R. Mitochondrial DNA damage and atherosclerosis. Trends Endocrinol. Metab. 25, 481–487 (2014).
Go, Y.M. et al. A key role for mitochondria in endothelial signaling by plasma cysteine/cystine redox potential. Free Radic. Biol. Med. 48, 275–283 (2010).
Bratic, A. & Larsson, N.G. The role of mitochondria in aging. J. Clin. Invest. 123, 951–957 (2013).
Jacob, C.O. et al. Lupus-associated causal mutation in neutrophil cytosolic factor 2 (NCF2) brings unique insights to the structure and function of NADPH oxidase. Proc. Natl. Acad. Sci. USA 109, E59–E67 (2012).
Vyshkina, T. et al. Association of common mitochondrial DNA variants with multiple sclerosis and systemic lupus erythematosus. Clin. Immunol. 129, 31–35 (2008).
Fuchs, T.A. et al. Novel cell death program leads to neutrophil extracellular traps. J. Cell Biol. 176, 231–241 (2007).
Fazzi, F. et al. TNFR1/phox interaction and TNFR1 mitochondrial translocation thwart silica-induced pulmonary fibrosis. J. Immunol. 192, 3837–3846 (2014).
West, A.P. et al. TLR signaling augments macrophage bactericidal activity through mitochondrial ROS. Nature 472, 476–480 (2011).
Sibley, C.T. et al. Assessment of atherosclerosis in chronic granulomatous disease. Circulation 130, 2031–2039 (2014).
Lekstrom-Himes, J.A., Kuhns, D.B., Alvord, W.G. & Gallin, J.I. Inhibition of human neutrophil IL-8 production by hydrogen peroxide and dysregulation in chronic granulomatous disease. J. Immunol. 174, 411–417 (2005).
Kraaij, M.D. et al. Induction of regulatory T cells by macrophages is dependent on production of reactive oxygen species. Proc. Natl. Acad. Sci. USA 107, 17686–17691 (2010).
Lee, K., Won, H.Y., Bae, M.A., Hong, J.H. & Hwang, E.S. Spontaneous and aging-dependent development of arthritis in NADPH oxidase 2 deficiency through altered differentiation of CD11b+ and TH/Treg cells. Proc. Natl. Acad. Sci. USA 108, 9548–9553 (2011).
Fernandez-Boyanapalli, R. et al. Impaired phagocytosis of apoptotic cells by macrophages in chronic granulomatous disease is reversed by IFN-γ in a nitric oxide–dependent manner. J. Immunol. 185, 4030–4041 (2010).
Meissner, F. et al. Inflammasome activation in NADPH oxidase defective mononuclear phagocytes from patients with chronic granulomatous disease. Blood 116, 1570–1573 (2010).
Schauer, C. et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat. Med. 20, 511–517 (2014).
Gane, E.J. et al. The mitochondria-targeted antioxidant mitoquinone decreases liver damage in a phase II study of hepatitis C patients. Liver Int. 30, 1019–1026 (2010).
Buyse, G.M. et al. Idebenone as a novel, therapeutic approach for Duchenne muscular dystrophy: results from a 12-month, double-blind, randomized placebo-controlled trial. Neuromuscul. Disord. 21, 396–405 (2011).
Tan, E.M. et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 25, 1271–1277 (1982).
Kuhns, D.B. et al. Residual NADPH oxidase and survival in chronic granulomatous disease. N. Engl. J. Med. 363, 2600–2610 (2010).
Olferiev, M., Lliguicota, M., Kirou, K.A. & Crow, M.K. Methods Mol. Biol. 1134, 131–150 (2014).
Ahmad, S., Ghosh, A., Nair, D.L. & Seshadri, M. Simultaneous extraction of nuclear and mitochondrial DNA from human blood. Genes Genet. Syst. 82, 429–432 (2007).
Ishikawa, H., Ma, Z. & Barber, G.N. STING regulates intracellular DNA-mediated, type-I interferon–dependent innate immunity. Nature 461, 788–792 (2009).
Boxio, R., Bossenmeyer-Pourié, C., Steinckwich, N., Dournon, C. & Nüsse, O. Mouse bone marrow contains large numbers of functionally competent neutrophils. J. Leukoc. Biol. 75, 604–611 (2004).
Carmona-Rivera, C., Simeonov, D.R., Cardillo, N.D., Gahl, W.A. & Cadilla, C.L. A divalent interaction between HPS1 and HPS4 is required for the formation of the biogenesis of lysosome-related organelle complex–3 (BLOC-3). Biochim. Biophys. Acta 1833, 468–478 (2013).
Acknowledgements
We thank X. Sun, L. Tanaka (both at University of Washington), and E. Moore (National Institute of Arthritis and Musculoskeletal and Skin Diseases; NIAMS) for technical assistance; W. Wang (University of Washington) for providing mouse mitochondria isolated from hearts; D. Kuhns (NIAID) for scientific input, and R. Siegel (NIAMS) for critical review of the manuscript. We also thank H.-W. Sun, M. Ward (both at NIAMS) and C. Spiekerman (University of Washington) for expert statistical advice. We also thank M. Gale for providing Tmem173-knockout mice. The study was supported by grants from the Washington Research Foundation, Leap for Lupus (K.B.E.), the Wenner-Gren Foundation, the foundation BLANCEFLOR Boncompagni-Ludovisi née Bildt (C.L.), and the Intramural Research Program at NIAMS/NIH (L.P.B., M.P., C.K.S., C.C.-R. and M.J.K.). The funding bodies had no part in the study design; the collection, analysis and interpretation of the data; the writing of the manuscript or the submission.
Author information
Authors and Affiliations
Contributions
All contributing authors have agreed to the submission of this manuscript for publication. K.B.E. and M.J.K. conceived the study, and analyzed and interpreted results. C.L., L.P.B., M.M.P., C.C.-R. and C.K.S. designed and performed experiments, analyzed data and interpreted results. S.S.D.R. and H.L.M. provided study materials and characterized the CGD cohort. J.A.L. participated in the design and interpretation of the in vitro data, as well as the critical review of the paper. C.L., L.P.B., K.B.E. and M.J.K. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and figures
Supplementary Figures 1–7 and Supplementary Table 1 (PDF 1860 kb)
Rights and permissions
About this article
Cite this article
Lood, C., Blanco, L., Purmalek, M. et al. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med 22, 146–153 (2016). https://doi.org/10.1038/nm.4027
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4027
This article is cited by
-
Vascular damage in systemic lupus erythematosus
Nature Reviews Nephrology (2024)
-
Neutrophil extracellular traps and neutrophilic dermatosis: an update review
Cell Death Discovery (2024)
-
Chronic endoplasmic reticulum stress in myotonic dystrophy type 2 promotes autoimmunity via mitochondrial DNA release
Nature Communications (2024)
-
SARS-CoV-2 primed platelets–derived microRNAs enhance NETs formation by extracellular vesicle transmission and TLR7/8 activation
Cell Communication and Signaling (2023)
-
Fasting-mimicking diet alleviates inflammatory pain by inhibiting neutrophil extracellular traps formation and neuroinflammation in the spinal cord
Cell Communication and Signaling (2023)