Abstract
Disease outcomes of HER2+ breast cancers have dramatically improved after targeted therapies, such as trastuzumab became available. The main mechanism of action of trastuzumab depends on immunoactivation, while immunosuppressive tumour phenotype has been linked to adverse outcomes. Current study included metastatic HER2+ breast cancer patients treated with trastuzumab (n = 40). Immunohistochemistry was conducted to detect nitric oxide synthase 2 (iNOS) expressing M1 polarized and CD163+ M2 polarized macrophages, FoxP3+ regulatory T-cells (Tregs), CD47 and indoleamine 2,3-dioxygenase 1 (IDO1). High number of iNOS+ M1-like macrophages, both in the center of the tumour (CT) and invasive margin (IM), was significantly associated with improved survival (p = 0.009) while high expression of IDO1 or CD47 in the malignant cells was associated with worsened prognosis (p = 0.018, p = 0.046). High number of CD163+ M2-like macrophages in the CT, but not in the IM, and high number of FoxP3+ Tregs in both locations showed non-significant tendencies towards poor prognosis. Moreover, high number of iNOS+ M1-like macrophages combined with high number of CD8+ T-cells in the CT was significantly associated with improved survival (p = 0.0003), and this combined marker predicted patient’s ability to remain progression-free without trastuzumab after responding to the therapy (p = 0.003). Current study highlights the role of M1 polarized macrophages alone and in combination with CD8+ cells in HER2+ breast cancer.
Similar content being viewed by others
Introduction
Human epidermal growth factor receptor 2 (HER2) gene is frequently amplified in breast cancers. Before introduction of modern HER2 targeted therapies such as trastuzumab, a monoclonal HER2 antibody, HER2 amplified disease was associated with high risk for relapse in localized disease and shortened overall survival in metastatic disease1,2,3,4,5. Trastuzumab functions by binding to the HER2 receptor and its main effect is mediated through antibody-dependent cellular cytotoxicity and antibody-dependent cellular phagocytosis6,7. Trastuzumab treatment has been shown to have several effects on the immune system, including increased natural killer (NK) cell proliferation and cytotoxicity, NK cell migration and adhesion, and increased phagocytosis of trastuzumab coated tumour cells by tumour-associated macrophages (TAMs), leading to increased tumour cell death7,8.
Tumour infiltrating lymphocytes have been associated with trastuzumab efficiency and improved survival in several cancers including breast cancer9,10,11. In our previous work with metastatic HER2+ breast cancer12, a high number of cytotoxic CD8+ T-cells in the center of the tumour, but not in the invasive margin, was significantly associated with the improved survival and patient’s ability to remain disease progression-free without trastuzumab after initially responding to the therapy.
Macrophages are known for their immunomodulatory effects. In a conventional manner, macrophages can be divided according to their phenotypes into M1- or M2-like states; M1-like macrophages have been linked to pro-inflammatory response, while M2-like macrophages are traditionally associated with wound repair and suppression of inflammation13. In many solid cancers, the number of TAMs is associated with prognosis and therapy response. In particular, TAMs with M1-like phenotype have been linked to good disease course while M2-like phenotype has been associated with adverse outcome, potentially through immunosuppression and the promotion of angiogenesis and tumour cell proliferation and invasion, which are critical prerequisite for metastatic cancer progression14.
In addition to M2-like macrophages, other cells of the immune system, such as regulatory T-cells (Tregs), can bare immunosuppressive functions. Tregs are essential for the development and maintenance of self-tolerance, preventing detrimental autoimmunity. On the other hand, Tregs have also been demonstrated to elicit protumour activity by suppressing antitumoural immune response. Tregs are in a reciprocal crosstalk with responding T-cells, M1/M2 macrophages and dendritic cells15. This crosstalk is mediated via contact-dependent cell-to-cell signalling and humoral signalling. Tregs are shown to utilize a variety of molecules to achieve immunosuppression, such as cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), IL-2 and IL-1016.
Expressed by a subset of tumours and immune cells, negative immune regulatory molecules may contribute to the suppression of anti-tumour immunity. Indoleamine 2,3-dioxygenase 1 (IDO1, also called IDO) is an intracellular enzyme catalysing the degradation of tryptophan, which is essential for immune tolerance17. IDO1 is expressed by a population of antigen presenting cells such as some dendritic cells and macrophages. Furthermore, many human tumours have been shown to express IDO1, enhancing the suppression of effector T-cells and NK cells. Conversely, IDO1 promotes the formation and activity of Tregs18,19,20,21,22,23,24. Another intriguing signalling molecule is CD47, which is expressed by variety of malignancies and negatively impacts phagocytosis25,26,27.
In this current study, we evaluated immunological markers in pre-treatment tumour samples of metastatic HER2+ breast cancer patients receiving trastuzumab therapy. Our primary hypothesis testing was set to assess the association between different macrophage subtypes, the density of FoxP3+ Tregs, and survival, while all other analyses were secondary. The results suggest that M1 polarized macrophages together with cytotoxic T-cells found in the center of the tumour are strongly positive and independent indicators for prognosis and predict long progression-free periods without trastuzumab.
Results
Patients and samples
We identified 54 patients who had received at least one doze of trastuzumab for metastatic breast cancer in 2009–2014 from the Oulu University Hospital pharmacy records. Of these patients, 41% had primary metastatic disease at the time of diagnosis and 59% had a relapsed disease. Analyses were limited to pre-treatment samples, which were available for 40 patients. The samples included 25 (62.5%) surgical specimens and 15 (37.5%) biopsy specimens. Furthermore, 12 patients of the 40 (30%) had a planned HER2 therapy interruption in tumour response.
The tumour samples were stained for inducible nitric oxide synthase (iNOS, M1 marker), CD163 (M2 marker), FoxP3 (Treg marker), CD47 and IDO1. Positivity for iNOS, CD163, and IDO1 was detected in a subset of tumour-associated macrophages (TAMs), while iNOS and IDO1 positivity was also seen in a subset (83% and 20%, respectively) of tumour cells (Fig. 1). FoxP3 positivity localized in the nuclei of a subset of lymphocytes, and membranous CD47 positivity was seen in tumour cells of 78% of tested cases (Fig. 1). Immune cells were analysed from the invasive margin (IM) and from the center of the tumour (CT) with a computer-assisted counting method previously used in colorectal cancers and HER2+ breast cancers12,28. CD47 and IDO1 staining in tumours was ranked from low (0) to high (3) intensities.
Representative examples of iNOS, CD163, FoxP3, CD47, and IDO1 immunohistochemistry. (a,b) iNOS positive and iNOS negative staining of the tumour cells. A subset of immune cells with macrophage-like morphology showed strong positivity. (c,d) High and low CD163 staining. A subset of immune cells with macrophage-like morphology showed strong cytoplasmic positivity. (e,f) High and low FoxP3 staining. Some lymphocytes had strong nuclear positivity. (g,h) CD47 positive and negative staining of the tumour cells. (I,j) IDO1 positive and negative staining of the tumour cells. In (j) but not in (i), some immune cells with macrophage-like morphology show strong immunoreaction. In all images, examples of positive immune cells are indicated with arrows. Scale bar = 100 µm.
Polarized macrophages predict survival
Differentially polarized TAMs were studied with iNOS and CD163, with a prespecified hypothesis that iNOS+ TAMs (M1-like phenotype) would be associated with improved prognosis, whereas CD163+ TAMs (M2-like phenotype) would be associated with adverse prognosis. iNOS+ and CD163+ cells were present in varying numbers in both IM and CT in all the tumours (Table 1). Kaplan-Meier estimates showed that a high number of iNOS+ M1-like macrophages in the IM (p = 0.009) and in the CT (p = 0.009) was significantly associated with an improved survival (Fig. 2a,b). In addition to M1-like macrophages, iNOS expression was detected in some tumour cells, but this did not provide any prognostic value (data not shown). The density of M2 polarized macrophages in the CT but not in the IM displayed a tendency towards poor survival, however, without statistical significance (Fig. 2c,d).
Survival analysis of metastatic HER2+ breast cancer in the presence of low or high infiltration of M1 and M2 polarized macrophages. (a,b) Kaplan-Meier estimates illustrate the association of M1 polarized macrophages with survival in IM (a) and CT (b) locations (cut-offs 42 and 37 cells/mm2). (c,d) Kaplan-Meier estimates illustrate the association of M2 polarized macrophages with survival in IM (c) and CT (d) locations (cut-offs 338 and 295 cells/mm2). Crosses mark censored events.
We also studied whether a combined M1 and M2 status could predict the patient outcome even better than the high number of M1-like macrophages alone. High number of M1-like macrophages together with low number of M2-like macrophages in both CT and IM was associated with improved survival (CT: p = 0.032, IM: p = 0.045), however, these associations were not more significant than the high number of M1-like macrophages alone.
Tumour immunosuppressive markers predict worsened survival
Next, we studied cells and molecules contributing to the immunosuppression in tumour microenvironment and their impact on survival. We hypothesized that high density of tumour infiltrating Tregs, and IDO1+ TAMs, as well as high tumour CD47 and IDO1 expression would be associated with adverse outcome.
We found that variable numbers of Tregs, identified with FoxP3 nuclear positivity, were present both in the IM and CT in each tumour (Table 1). In the survival analysis, a high number of Tregs both in the IM and CT showed a tendency towards worsened survival (Fig. 3a,b), however not reaching a statistical significance.
Survival analysis of metastatic HER2+ breast cancer in the presence of low or high infiltration of regulatory T-cells. Kaplan-Meier estimates demonstrate the association of regulatory T-cells with survival in the IM (a) and CT (b) locations (cut-offs 145 and 92 cells/mm2). Crosses mark censored events.
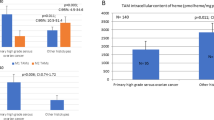
Next, we evaluated potential immunosuppressive factors expressed by the tumour cells. Low CD47 intensity (0–1) in the tumour was associated with improved survival, whereas high CD47 intensity (2–3) predicted worsened survival (p = 0.046, Fig. 4a). Similar to CD47, tumour intensity of IDO1, a broadly studied immunosuppressive molecule, was used to group the samples into two categories (0–1, 2–3). IDO1 analysis was limited only to 25 tumours because of limited tumour sample availability. The results showed that high tumour IDO1 intensity was associated with poor survival (p = 0.018, Fig. 4b). IDO1 expression was observed also in a subset of macrophages, both in the IM and CT, but their density showed no association with survival (not shown). We also performed a combined analysis of the CD47 and IDO1 tumour cell intensities using three-tiered classification; high intensity of both markers, high intensity of only one marker, low intensity of both markers. A significant association was seen between the low intensity of both CD47 and IDO1 with improved survival (p = 0.037). However, in a multivariate analysis only IDO1 remained as an independent prognostic factor (CD47: HR 1.973, 95% CI 0.725–5.369; p = 0.183, IDO1: HR 3.333, 95% CI 1.108–10.031; p = 0.032).
High number of tumour CD8 cells and M1 macrophages independently predict survival and long trastuzumab-free periods
We have previously shown that a high number of CD8+ cytotoxic T-cells in the center of the tumour predicts better survival in metastatic disease12. Since in the current study, the quantity of iNOS+ M1-like macrophages was the most promising indicator for improved survival, we wanted to assess if combining these two markers would enhance the prognostic value compared to single markers alone. A high number of CD8+ T-cell in the CT combined with high number of iNOS+ M1-like macrophages in the IM (p = 0.0003, Fig. 5a) or CT (p = 0.0003, Fig. 5b) was significantly associated with improved survival compared to positivity by single marker. On the contrary, patients with both low CD8+ T-cells in the CT and low iNOS+ M1-like macrophages in the IM or CT had worsened survival compared to patients with single positive tumours (Fig. 5).
Survival analysis of metastatic HER2+ breast cancer in the presence of low, intermediate or high infiltration of both M1 polarized macrophages and CD8+ T-cells. (a) Kaplan-Meier estimate illustrates the association between M1 macrophages in the IM combined with CD8+ T-cells in the CT and survival. (b) Kaplan-Meier estimate illustrates the association between M1 macrophages in the CT combined with CD8+ T-cells in the CT and survival. Crosses mark censored events.
We further analysed whether CD8+ T-cells in the CT and iNOS+ M1-like macrophages in the IM or CT would remain as independent prognostic factors in a multivariate analysis. When the density of CD8+ T-cells in the CT (HR 2.923, 95% CI 1.305–6.546; p = 0.009) and M1-like macrophages in the IM (HR 3.078, 95% CI 1.298–7.298; p = 0.011) were included in the same model, both parameters remained as independent prognostic factors. Similarly, when the density of CD8+ T-cells in the CT (HR 2.957, 95% CI 1.336–6.543; p = 0.007) and M1-like macrophages in the CT (HR 2.813, 95% CI 1.302–6.077; p = 0.009) were included in the same model both remained as independent prognostic factors.
Our previous results showed that a high number of CD8+ T-cells in the center of the tumour predicts patient’s ability to remain disease progression-free without trastuzumab after responding to the therapy12. We wanted to study whether the density of iNOS+ M1-like macrophages in the IM or CT combined with CD8+ T-cells in the CT would predict the length of trastuzumab free-periods in metastatic disease better than CD8+ T-cells alone. A high number of CD8+ T-cells in the CT together with a high number of M1-like macrophages in the IM (p = 0.003) or CT (p = 0.003) was strongly associated with a long trastuzumab free-periods after response (Fig. 6a,b).
M1 polarized macrophages and CD8+ T-cells predict the length of trastuzumab-free period after response. (a) Kaplan-Meier estimate demonstrates the association of combined M1 IM and CD8 CT status with the trastuzumab discontinuation length. (b) Kaplan-Meier estimate demonstrates the association of the combined M1 CT and CD8 CT status with the trastuzumab discontinuation length. Crosses mark censored events.
Discussion
The development of HER2 targeting antibodies, such as trastuzumab, have revolutionized the treatment and outcomes of HER2 positive breast cancer patients3,4,5. However, trastuzumab is still administered according to the HER2 status only due to a lack of predictive factors for trastuzumab sensitivity and resistance. Since the mechanisms of action of trastuzumab is related to both signal inhibition and immune activation29, trastuzumab responses can be affected by the altered signalling pathways and the immunological status of the tumour. Some mechanisms for the trastuzumab resistance have been described, such as compromised host immunoactivation, a shorter variant of HER2 (p95), and altered expressions/mutations of PI3KCA and PTEN30. We have previously shown a strong association between high number of CD8+ T-cells in the center of the tumour and improved survival and long trastuzumab-free periods in metastatic HER2+ breast cancer12. In the current study we investigated additional immunological markers which could be used together with CD8 for predicting the prognosis and trastuzumab responses in metastatic HER2 positive breast cancer.
Macrophages have been widely studied in different cancer types and their presence in the tumour microenvironment is known to have clinical relevance31. Current research of cancer immunology is leaning towards defining the role of macrophage polarization and its impact on the disease course and outcome. M2 polarized TAMs are known to have immunosuppressive functions and, indeed, M2 polarized macrophages have been correlated to poor prognosis in various solid cancers including breast, ovarian, gastric and colorectal cancers32,33,34,35. Conversely, antitumour M1 polarized macrophages are linked to favourable prognosis in lung, ovarian, gastric and hepatocellular cancers34,36,37,38. Little is known about the clinical importance of macrophages in HER2+ breast cancer, especially about M1 polarized macrophages and their prognostic role. We found that high density of iNOS+ M1-like macrophages predicted improved survival in our cohort of HER2+ breast cancer, which is consistent with other studies in other types of cancer. Our data highlights the potential of M1 polarized macrophages as a prognostic marker in metastatic HER2+ breast cancer. We have previously shown that prognostic role of CD8+ T-cells is limited to the center tumour location only12 while for TAMs, the number but not the spatial distribution, is significant. This might reflect the role of macrophages as a general regulator of tumour immunology. Our results indicate that therapeutic approaches targeting macrophage polarization in HER2+ breast cancer could represent a reasonable target for further investigation.
The function of trastuzumab is mainly mediated by immunoactivation29,39. Mechanistically, immunological function of tumour directed antibodies is thought to be principally caused by NK cell-mediated antibody-dependent cellular cytotoxicity. Previous studies with HER2 positive breast cancer have demonstrated increased NK cell infiltration and activation in tumours after administration of trastuzumab and its relation to good responses39,40,41,42. A very recent work43 has highlighted the effects of macrophages on trastuzumab responses. Trastuzumab enhances antibody-dependent cellular phagocytosis by macrophages leading to upregulation of IDO1 and PD-L1 and immunosuppression. This finding is counterintuitive considering to the well-established benefit of monoclonal antibodies in cancer therapy and raises a question whether macrophages could be used as a predictive marker and therapeutic target. Our results favour the importance of macrophages for tumour immunology and their therapeutic exploration in HER2+ cancers.
Upregulation of IDO1 has been linked to high number of regulatory T-cells in tumours and increased M2/M1 ratio22,44,45 while high CD47 has been linked to inhibition of macrophage-mediated phagocytosis25,27 both leading to tumour immunosuppression. Our results also showed that low IDO1 and CD47 in tumour cells associated with improved prognosis, further supporting the importance of TAMs. A recent study46 has shown that blocking CD47 in addition to CD20 can have substantial clinical effect in lymphomas with very favourable safety profile. It is still early to conclude whether macrophage-mediated phagocytosis has strong immunoactivating or immunosuppressive function in tumours.
Trastuzumab still remains the gold standard for the treatment of HER2 positive breast cancer but acquired resistance develops in most patients with metastatic disease and some are primary refractory for the treatment. Currently, the use of trastuzumab in cancer therapy is determined by HER2 status only. In the era of personalized medicine, patient selection for the treatment should be better optimized. The results by us and others47 have clearly defined that immune cells have crucial impact on the disease course, and characterizing the amount and function of these cells could provide a new aspect for treatment selection. The patients with favourable tumour immunoprofile (high tumour infiltrating CD8+ T-cells and iNOS+ M1 TAMs in the CT, and low tumour expression of CD47 and IDO1) might be treated with less intensive manner and remain progression-free during trastuzumab interruption while patients with non-favourable immunoprofile are candidates for experimental immunotherapeutic approaches. However, these hypotheses need to be confirmed in subsequent larger prospective studies.
Our study had some limitations. The number of tumour samples was low, and patients were retrospectively collected from a single academic cancer center. Furthermore, tumour material of the study consisted of patients, all of whom were treated with trastuzumab, making evaluation of predictive values more difficult. Identification of immune cell phenotypes was carried out with single markers only, which does not acknowledge for the complexity of the phenotypically diverse group of macrophages48. However, well characterized and widely used markers were selected for the study. Multiple hypotheses were tested in this observational study, which increases the risk of type 1 statistical error. Therefore, we interpreted the findings with p near 0.05 with caution, and the significance of the validation of these findings in an independent study with larger patient material needs to be emphasized.
In conclusion, our study investigated the role of immunological markers in metastatic HER2+ breast cancer patients receiving trastuzumab therapy. The main results suggest that iNOS+ M1- like macrophages together with cytotoxic T-cells are independent indicators for prognosis and predict long progression-free periods without trastuzumab.
Materials and Methods
Patient data
The patients were retrospectively identified from the pharmacy records of Oulu University Hospital as previously12. All patients who had received at least one dose of intravenous trastuzumab in 2009–2014 for the treatment of metastatic breast cancer were selected (n = 54). The study was limited to those patients who had adequate pre-treatment samples available (n = 40). HER2 positivity was characterized by the presence of HER2 amplification in chromogenic in situ hybridization. The patient data collection and tumour analysis were carried out under permits from the medical director of Oulu University Hospital (study no. 60/2015), the Northern Osthrobothnia Hospital District ethical committee (114/2011, amendment 23.02.2015) and National Supervisory Authority for Welfare and Health (9850/05.01.00.06/2010). According to the national legislation of Finland, tissues gathered for diagnostic purposes can be used in scientific studies without an informed consent from the patient and therefore it was not obtained, and it is not relevant for the study. All the experiments were performed in accordance with relevant guidelines and regulations.
The patients’ age, date of diagnosis, date of metastatic disease, adjuvant/metastatic treatment regimens, treatment durations and therapy responses among other characteristics described earlier12,49 were collected from the electronic patient records. Survival in metastatic disease was calculated from the time of histological or radiological identification of metastatic disease to death or end of follow-up. Patients whose HER2 therapy was interrupted were characterized by having a planned HER2 therapy interruption in connection with a response lasting >12 months or with a response plus severe suspected HER2 therapy-related adverse events. HER2 therapy discontinuation length was defined from the date of the last administration of trastuzumab (in the longest HER2 therapy discontinuation period) to the date of drug re-initiation, death, or end of follow-up. The clinical characteristics of the patients have earlier been described in more detail49.
Immunohistochemistry and immune cell counting
Immunohistochemistry was conducted on 3.5 µm sections cut from paraffin-embedded specimens. The sections were deparaffinized in HistoClear (IDO1) or xylene and rehydrated through graded alcohols. Antigen retrieval was conducted in a microwave oven with citrate buffer (pH6; IDO1) or Tris-EDTA buffer (pH9; iNOS, CD163, FoxP3, CD47) at 800 W for 2 min and at 150 W for 10 (IDO1) or 15 min (other markers). Endogenous peroxidase activity was neutralized in 3% H202-aqua solution or in Dako REAL peroxidase blocking solution for 5 min. The tissue samples were incubated with primary antibodies (IDO1, Cell Signaling Technology, rabbit monoclonal, clone D5J4E™, dilution 1:400, overnight at + 4 °C; iNOS, Enzo Life Sciences, rabbit polyclonal, ADI-905–431–1, dilution 1:200, 60 min at RT; CD163, NeoMarkers, mouse monoclonal, clone 10D6, dilution 1:200, 30 min at RT; FoxP3, Abcam, mouse monoclonal, clone 236 A/E7, dilution 1:100, 30 min at RT; CD47, Atlas Antibodies, rabbit polyclonal, HPA044659, dilution 1:150, 60 min at RT). Bound antibodies were detected using the EnVisionTM (Dako) system. Diaminobenzidine (DAB) was used as the chromogen and hematoxylin as the counterstain. CD8 (Novocastra, mouse monoclonal, clone 4B11, dilution 1:200) staining used in the current study was performed earlier12.
For the analysis of immunohistochemistry, the sections were scanned with Aperio AT2 image-capturing device (Leica Biosystems). Imagescope (Aperio Technologies) software, version 11.2 was used to view the scanned images and capture images from the center of the tumour (CT) and the invasive margin (IM) for immune cell counting. The criteria for the different tumour locations are previously described12. The intensity of tumour cell immunoreaction for iNOS (cytoplasmic), IDO1 (cytoplasmic), or CD47 (membranous) was evaluated as negative (0), weak (1), moderate (2), or strong (3)50. The immune cells were counted using an earlier described and validated computer-assisted counting method28,51 that utilizes ImageJ, a freeware image analysis software52. Final counts presented in this manuscript are the average cell densities for each tumour area.
Statistics
IBM SPSS Statistics 24.0 for Windows (IBM Corporation, Armonk, NY, USA) was applied for statistical analysis. The reported p-values are from two-sided chi-square tests. Receiver operating characteristics (ROC) analysis for the whole patient material was used to determine optimal cut-off scores of iNOS, CD163, FoxP3 and IDO1 for discriminating the survivors from the non-survivors. In the survival analyses, scores over the cut-off value were defined as “high” and the scores below were defined as “low”. Survival was analysed by using the Kaplan-Meier method with the log-rank test. Multivariate analysis was performed using Cox regression analysis. Probability values below 0.05 were considered significant.
Data Availability
The raw data used in the analyses of the current study is not publicly available due to legislative issues concerning the privacy of the patients.
References
Slamon, D. J. et al. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235, 177–182 (1987).
Gonzalez-Angulo, A. M. et al. High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J. Clin. Oncol. 27, 5700–5706 (2009).
Marty, M. et al. Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: The M77001 study group. J. Clin. Oncol. 23, 4265–4274 (2005).
Swain, S. M. et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. New Engl. J. Med. 372, 724–734 (2014).
Von Minckwitz, G. et al. Trastuzumab beyond progression in human epidermal growth factor receptor 2-positive advanced breast cancer: A German Breast Group 26/Breast International Group 03-05 study. J. Clin. Oncol. 27, 1999–2006 (2009).
Hudis, C. A. Trastuzumab - Mechanism of action and use in clinical practice. New Engl. J. Med. 357, 39–51 (2007).
Cooley, S., Burns, L. J., Repka, T. & Miller, J. S. Natural killer cell cytotoxicity of breast cancer targets is enhanced by two distinct mechanisms of antibody-dependent cellular cytotoxicity against LFA-3 and HER2/neu. Exp. Hematol. 27, 1533–1541 (1999).
Shi, Y. et al. Trastuzumab triggers phagocytic killing of high HER2 cancer cells in vitro and in vivo by interaction with Fcγ receptors on macrophages. J. Immunol. 194, 4379–4386 (2015).
Loi, S. et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: Results from the FinHER trial. Ann. Oncol. 25, 1544–1550 (2014).
Gennari, R. et al. Pilot study of the mechanism of action of preoperative trastuzumab in patients with primary operable breast tumors overexpressing HER2. Clin. Cancer Res. 10, 5650–5655 (2004).
Salgado, R. et al. Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: A secondary analysis of the NeoALTTO trial. JAMA Oncol. 1, 448–455 (2015).
Honkanen, T. J. et al. Prognostic and predictive role of spatially positioned tumour infiltrating lymphocytes in metastatic HER2 positive breast cancer treated with trastuzumab. Sci. Rep. 7 (2017).
Williams, C. B., Yeh, E. S. & Soloff, A. C. Tumor-associated macrophages: unwitting accomplices in breast cancer malignancy. NPJ Breast Cancer. 2, https://doi.org/10.1038/npjbcancer.2015.25. Epub 2016 Jan 20 (2016).
Biswas, S. K., Allavena, P. & Mantovani, A. Tumor-associated macrophages: Functional diversity, clinical significance, and open questions. Semin. Immunopathol. 35, 585–600 (2013).
Roychoudhuri, R., Eil, R. L. & Restifo, N. P. The interplay of effector and regulatory T cells in cancer. Curr. Opin. Immunol. 33, 101–111 (2015).
Nishikawa, H. & Sakaguchi, S. Regulatory T cells in cancer immunotherapy. Curr. Opin. Immunol. 27, 1–7 (2014).
Mellor, A. L. & Munn, D. H. IDO expression by dendritic cells: Tolerance and tryptophan catabolism. Nat. Rev. Immunol. 4, 762–774 (2004).
Munn, D. H. et al. Potential regulatory function of human dendritic cells expressing indoleamine 2,3-dioxygenase. Science 297, 1867–1870 (2002).
Theate, I. et al. Extensive profiling of the expression of the indoleamine 2,3-dioxygenase 1 protein in normal and tumoral human tissues. Cancer Immunol. Res. 3, 161–172 (2015).
Uyttenhove, C. et al. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat. Med. 9, 1269–1274 (2003).
Della Chiesa, M. et al. The tryptophan catabolite L-kynurenine inhibits the surface expression of NKp46- and NKG2D-activating receptors and regulates NK-cell function. Blood 108, 4118–4125 (2006).
Baban, B. et al. IDO activates regulatory T cells and blocks their conversion into Th17-like T cells. J. Immunol. 183, 2475–2483 (2009).
Munn, D. H. et al. Inhibition of T cell proliferation by macrophage tryptophan catabolism. J. Exp. Med. 189, 1363–1372 (1999).
Liu, X. et al. Selective inhibition of IDO1 effectively regulates mediators of antitumor immunity. Blood 115, 3520–3530 (2010).
Willingham, S. B. et al. The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc. Natl. Acad. Sci. USA 109, 6662–6667 (2012).
Weiskopf, K. et al. CD47-blocking immunotherapies stimulate macrophage-mediated destruction of small-cell lung cancer. J. Clin. Invest. 126, 2610–2620 (2016).
Jaiswal, S. et al. CD47 Is Upregulated on Circulating Hematopoietic Stem Cells and Leukemia Cells to Avoid Phagocytosis. Cell 138, 271–285 (2009).
Väyrynen, J. P. et al. An improved image analysis method for cell counting lends credibility to the prognostic significance of T cells in colorectal cancer. Virchows Arch. 460, 455–465 (2012).
Nami, B., Maadi, H. & Wang, Z. Mechanisms underlying the action and synergism of trastuzumab and pertuzumab in targeting HER2-positive breast cancer. Cancers 10 (2018).
Gagliato, D. M., Jardim, D. L. F., Marchesi, M. S. P. & Hortobagyi, G. N. Mechanisms of resistance and sensitivity to anti-HER2 therapies in HER2+ breast cancer. Oncotarget 7, 64431–64446 (2016).
Fridman, W. H., Zitvogel, L., Sautès-Fridman, C. & Kroemer, G. The immune contexture in cancer prognosis and treatment. Nat. Rev. Clin. Oncol. 14, 717–734 (2017).
Medrek, C., Pontén, F., Jirström, K. & Leandersson, K. The presence of tumor associated macrophages in tumor stroma as a prognostic marker for breast cancer patients. BMC Cancer 12 (2012).
Lan, C. et al. Expression of M2-polarized macrophages is associated with poor prognosis for advanced epithelial ovarian cancer. Technol. Cancer Res. Treat. 12, 259–267 (2013).
Zhang, H. et al. Infiltration of diametrically polarized macrophages predicts overall survival of patients with gastric cancer after surgical resection. Gastric Cancer 18, 740–750 (2015).
Herrera, M. et al. Cancer-associated fibroblast and M2 macrophage markers together predict outcome in colorectal cancer patients. Cancer Sci. 104, 437–444 (2013).
Ma, J. et al. The M1 form of tumor-associated macrophages in non-small cell lung cancer is positively associated with survival time. BMC Cancer 10 (2010).
Zhang, M. et al. A high M1/M2 ratio of tumor-associated macrophages is associated with extended survival in ovarian cancer patients. J. Ovarian Res. 7 (2014).
Dong, P. et al. CD86+/CD206+, diametrically polarized tumor-associated macrophages, predict hepatocellular carcinoma patient prognosis. Int. J. Mol. Sci. 17 (2016).
Petricevic, B. et al. Trastuzumab mediates antibody-dependent cell-mediated cytotoxicity and phagocytosis to the same extent in both adjuvant and metastatic HER2/neu breast cancer patients. J. Transl. Med. 11 (2013).
Arnould, L. et al. Trastuzumab-based treatment of HER2-positive breast cancer: An antibody-dependent cellular cytotoxicity mechanism? Br. J. Cancer 94, 259–267 (2006).
Varchetta, S. et al. Elements related to heterogeneity of antibody-dependent cell cytotoxicity in patients under trastuzumab therapy for primary operable breast cancer overexpressing Her2. Cancer Res. 67, 11991–11999 (2007).
Tian, X. et al. Herceptin enhances the antitumor effect of natural killer cells on breast cancer cells expressing human epidermal growth factor receptor-2. Front. Immunol. 8 (2017).
Su, S. et al. Immune Checkpoint Inhibition Overcomes ADCP-Induced Immunosuppression by Macrophages. Cell 175, 457.e23 (2018).
Wainwright, D. A. et al. IDO expression in brain tumors increases the recruitment of regulatory T cells and negatively impacts survival. Clin. Cancer Res. 18, 6110–6121 (2012).
Wang, X.- et al. The role of indoleamine 2,3-dioxygenase (IDO) in immune tolerance: Focus on macrophage polarization of THP-1 cells. Cell. Immunol. 289, 42–48 (2014).
Advani, R. et al. CD47 Blockade by Hu5F9-G4 and Rituximab in Non-Hodgkin’s Lymphoma. N. Engl. J. Med. 379, 1711–1721 (2018).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19, 40–50 (2018).
Murray, P. J. et al. Macrophage Activation and Polarization: Nomenclature and Experimental Guidelines. Immunity 41, 14–20 (2014).
Moilanen, T., Mustanoja, S., Karihtala, P. & Koivunen, J. P. Retrospective analysis of HER2 therapy interruption in patients responding to the treatment in metastatic HER2+ breast cancer. ESMO Open 2 (2017).
Zlobec, I., Terracciano, L., Jass, J. R. & Lugli, A. Value of staining intensity in the interpretation of immunohistochemistry for tumor markers in colorectal cancer. Virchows Arch. 451, 763–769 (2007).
Väyrynen, J. P. et al. Detailed analysis of inflammatory cell infiltration in colorectal cancer. The British Journal of Cancer 109, 1839–1847 (2013).
Abràmoff, M. D., Magalhães, P. J. & Ram, S. J. Image processing with imageJ. Biophoton Int. 11, 36–41 (2004).
Acknowledgements
The authors express their gratitude to Ms Riitta Vuento and Ms Anne Bisi for their assistance in the preparation of the study material. This work was supported by University of Oulu, Oulu University Hospital, Cancer Foundation Finland sr. (J.P.K.) and Ida Montin foundation (T.J.H.).
Author information
Authors and Affiliations
Contributions
J.P.K., M.M., J.P.V., P.K. and T.J.H. designed and coordinated the work. J.P.V., J.P.K. and T.J.H. gathered data. J.P.K., T.J.H. and A.T. carried out statistical analysis. All the authors participated in analysis and interpretation of the data, and drafted, read, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Honkanen, T.J., Tikkanen, A., Karihtala, P. et al. Prognostic and predictive role of tumour-associated macrophages in HER2 positive breast cancer. Sci Rep 9, 10961 (2019). https://doi.org/10.1038/s41598-019-47375-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-47375-2
This article is cited by
-
Immunohistochemical characterisation of the immune landscape in primary uveal melanoma and liver metastases
British Journal of Cancer (2023)
-
Prognostic significance of crown-like structures to trastuzumab response in patients with primary invasive HER2 + breast carcinoma
Scientific Reports (2022)
-
Immune cell profiles of metastatic HER2-positive breast cancer patients according to the sites of metastasis
Breast Cancer Research and Treatment (2022)
-
Clinical trial data and emerging strategies: HER2-positive breast cancer
Breast Cancer Research and Treatment (2022)
-
Roles of IFN-γ in tumor progression and regression: a review
Biomarker Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.